Юбилей
Original studies
Background: The main components of mineral metabolism can influence non-classical target organs such as adipose tissue, pancreas, vascular wall. The «metabolic» effects of parathyroid hormone (PTH) and other participants of phosphorus-calcium metabolism in the hyperfunction of parathyroid glands remain unclear. The study of disorders of carbohydrate, fat and other types of metabolism in primary hyperparathyroidism (PHPT) will help to develop effective measures for prophylaxis and treatment of the patients in order to improve the quality and life span of the population.
Aim: To study the main parameters of metabolism in young patients with an active stage of PHPT before surgical treatment.
Materials and methods: A one-stage comparative study of young patients with PHPT and healthy volunteers matched by sex, age and body mass index (BMI) was carried out. The participants underwent a comprehensive biochemical and hormonal examination, a hyperinsulinemic euglycemic clamp and a bioimpedance analysis of the body composition.
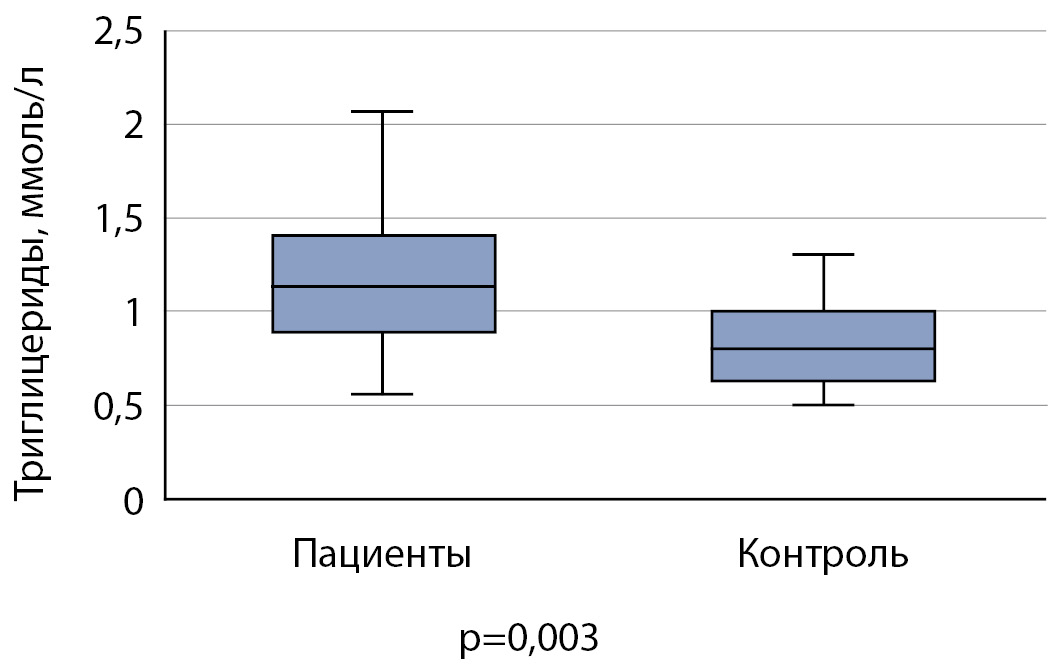
Results: 21 patients with PHPT and 18 healthy volunteers were included in the study. Patients with PHPT have higher level of serum triglycerides (p=0.003) without statistically differences of the main carbohydrate and purine parameters comparing with the control group. Visceral obesity were revealed in 42.9% of patients, including those with a normal BMI. Insulin resistance in the PHPT group was noted in 52.4% of cases, while the M-index was statistically lower than in the control subgroup (p=0.008), despite of the comparable body composition of the participants. The M-index showed a positive correlation with blood phosphorus level (p=0.010) only in the general group. Statistically positive correlations of PTH, albumin-corrected calcium and osteocalcin with triglyceride levels, calcium with fasting glycaemia, and PTH with uric acid levels were determined.
Conclusion: PHPT is associated with insulin resistance in patients that is the main risk factor for the development of serious carbohydrate and fat disorders. The positive correlation of PTH and blood calcium levels with triglycerides, as well as the tendency to hypertriglyceridemia comparing with healthy volunteers, suggest the disease effect on the development of dyslipidemia.
Background: Aldosterone-producing adrenocortical adenoma (APA) is responsible for the majority of cases clinically diagnosed as primary aldosteronism. Aldosterone synthase (CYP11B2) is one of the enzymes that play essential roles in aldosterone synthesis and is involved in the pathogenesis of primary aldosteronism. Recent studies have demonstrated that various factors influence the expression and function of CYP11B2 in APA. In particular, somatic mutations, such as gain-of-function and loss-of-function mutations have been identified in several genes, each of which encodes a pivotal protein that affects the calcium signaling pathway, the expression of CYP11B2, and aldosterone production. On the other hand, CYP11B2 also catalyzes the conversion of cortisol to 18-hydroxycortisol and subsequently converts 18-hydroxycortisol to 18-oxocortisol. The article also discusses the clinical significance of 18-oxocortisol, an important biomarker for the diagnosis of primary aldosteronism. Somatic mutations in aldosterone-driver genes are strongly associated with CYP11B2 expression and have been only detected in the CYP11B2-positive tumor area, that indicating heterogeneous expression of CYP11B2 in tumor.
Aim: to assess the functional heterogeneity of adrenal tumors in primary aldosteronism
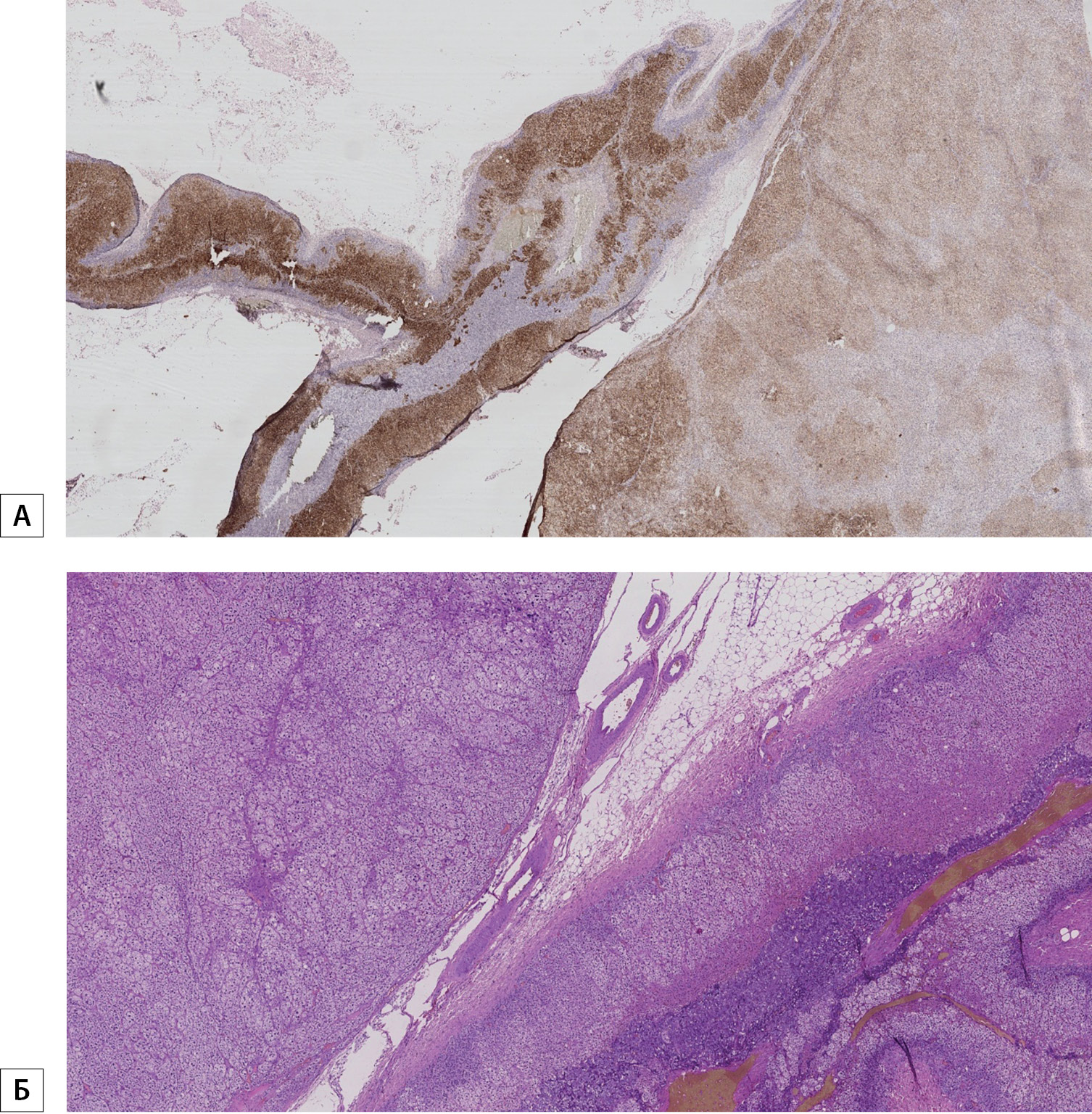
Materials and methods: Retrospective evaluation adrenal tumors from patients with primary aldosteronism (n=20). According to CT unilateral macrohyperplasia was detected in 19 patients (95% of total), all of them were confirmed to have unilateral hyperproduction of aldosterone according to AVS. Selected tumors werestained with anty-CYP11B2 antibody. We evaluated the CYP11B2 expression in the adenoma and in the adjacent adrenal cortex.
Results: Immunohistochemistry studies of the resected adrenals from 20 patients with PA operated due to unilateral production of aldosterone using CYP11B2 staining showed that 10 of those with an adenoma on CT scanning showed CYP11B2 staining in the adenoma. Furthermore, 5 cases of an unilateral adenoma, showed CYP11B2 staining in the adjacent adrenal cortex and an absence of staining for CYP11B2 in the adenoma. 5 cases showed CYP11B2 expression is heterogeneously immunolocalized throughout the tumor area.
Conclusion: Thus, the functional heterogeneity of adrenal tumors in primary aldosteronism has been proven. It is necessary to compare the data of immunohistochemical studies on the expression of CYP11B2 with the indicators of the level of 18-hydroxycortisol, 18-oxocortisol.
Background: Obesity is considered a global epidemic and is one of the most significant medical and social problems. Research in recent years shows that in 25-45% of cases of obesity, polycystic ovary syndrome (PCOS) is detected. The influence of obesity on the pathogenesis of metabolic disorders in this category of patients remains controversial
Aims: to determine the frequency and structure of metabolic disorders in obese women in combination with polycystic ovary syndrome (PCOS).
Materials and methods: A single-center cross-sectional sample survey of women of reproductive age was conducted. The study included clinical anthropometry with measurement of body weight, height, waist circumference (OT) and hip circumference (OB), followed by calculation of body mass index (BMI) and OT/OB ratio, and measurement of blood pressure (BP). A biochemical blood test was performed, the hormonal status was examined, and an ultrasound examination of the pelvic organs was performed.
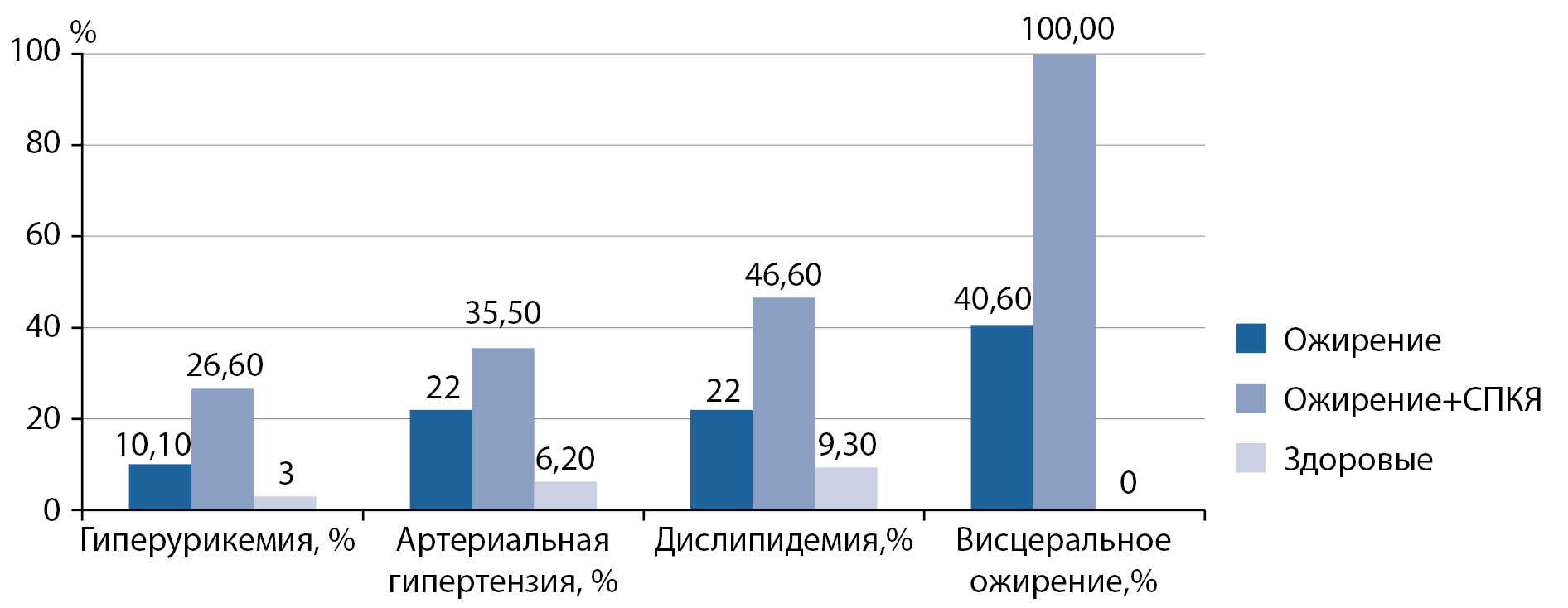
Results: A survey of 136 women of reproductive age was conducted. Group 1 included obese women without PCOS (59 patients), group 2 included obese women in combination with PCOS (45 patients), and the control group included 38 healthy women. Group 1 included obese women without PCOS (59 patients), and group 2 included obese women with PCOS (45 patients), in the control group — 38 healthy women. Among group 2 patients, dyslipidemia, visceral obesity, arterial hypertension, insulin resistance, hyperinsulinemia, and hyperuricemia were significantly more common (p<0,05). Correlations between BMI and triglycerides, testosterone and total cholesterol were found (p<0,05). Obese and PCOS patients had significantly higher levels of C-reactive protein(CRP), fibrinogen, anti-Müllerian hormone (AMH), and hepatic transaminases (p<0,05). Vitamin D deficiency was detected in 13,2% of patients, and insufficiency — in 22,7% of patients. There is a statistically significant correlation between the level of 25 (OH)D and indicators of BMI, follicle-stimulating hormone, luteinizing hormone (p<0,05), the level of AMH (p=0,008).
Conclusions: A high frequency of metabolic disorders in obese women in combination with PCOS has been identified, which necessitates early screening, diagnosis and treatment of these disorders to strengthen reproductive health and prevent chronic non-communicable diseases.
Background: Considering the influence of visceral obesity on male infertility, the investigation of ejaculate quality indicators under obesity treatment is relevant.
Objective: Evaluation of ejaculate quality indicators by obesity treatment with liraglutide in andrologically healthy men with infertility and post-pubertal visceral obesity.
Methods: Infertile men with post-pubertal alimentary visceral obesity were included in a pilot observational prospective study. All patients were given recommendations for body weight loss (hypocaloric diet, daily aerobic physical activity) as well as an average daily dose of liraglutide 2.4 [2.4; 3.0] mg. Evaluation of waist circumference, antioxidant activity of ejaculate, spermogram was carried out initially and after 6 months. The differences were considered statistically significant at p <0.005.
Results: The body weight decrease was -11.7 [12.4; 11.0]%, the waist circumference decrease was 8 [12; 7] cm. In dynamics, increased content of living sperm in ejaculate from 92 [90; 95]% to 95 [92; 98]%, morphologically normal forms from 5 [3; 6]% to 6 [3; 8]%, mobility of A + B from 25 [15; 36] to 35 [19; 52]%, seminal antioxidant capacity, a decrease in reactive oxygen forms in the neat ejaculate were statistically significant. Increasing the sperm count in 1 ml and decreasing reactive oxygen forms in the washed ejaculate did not reach statistical significance.
Conclusion: Ejaculate quality indicators improved by the complex obesity therapy with liraglutide in young andrologically healthy men with postpubertal visceral obesity.
Background: The use of testosterone replacement therapy (TRT) is widespread. Despite the positive changes, such as: an increase in testosterone levels, an improvement in erectile function and an increase in libido, it is possible to develop a negative manifestation — hyperestrogenism. To date, there are no studies assessing the prevalence of hyperestrogenism in the presence of TRT.
Aim: To study the reliability of an increase in total testosterone and estradiol levels and changes in total weight, body mass index (BMI), waist circumference (WC) and hips (OB), depending on the type of TRT and hCG therapy.
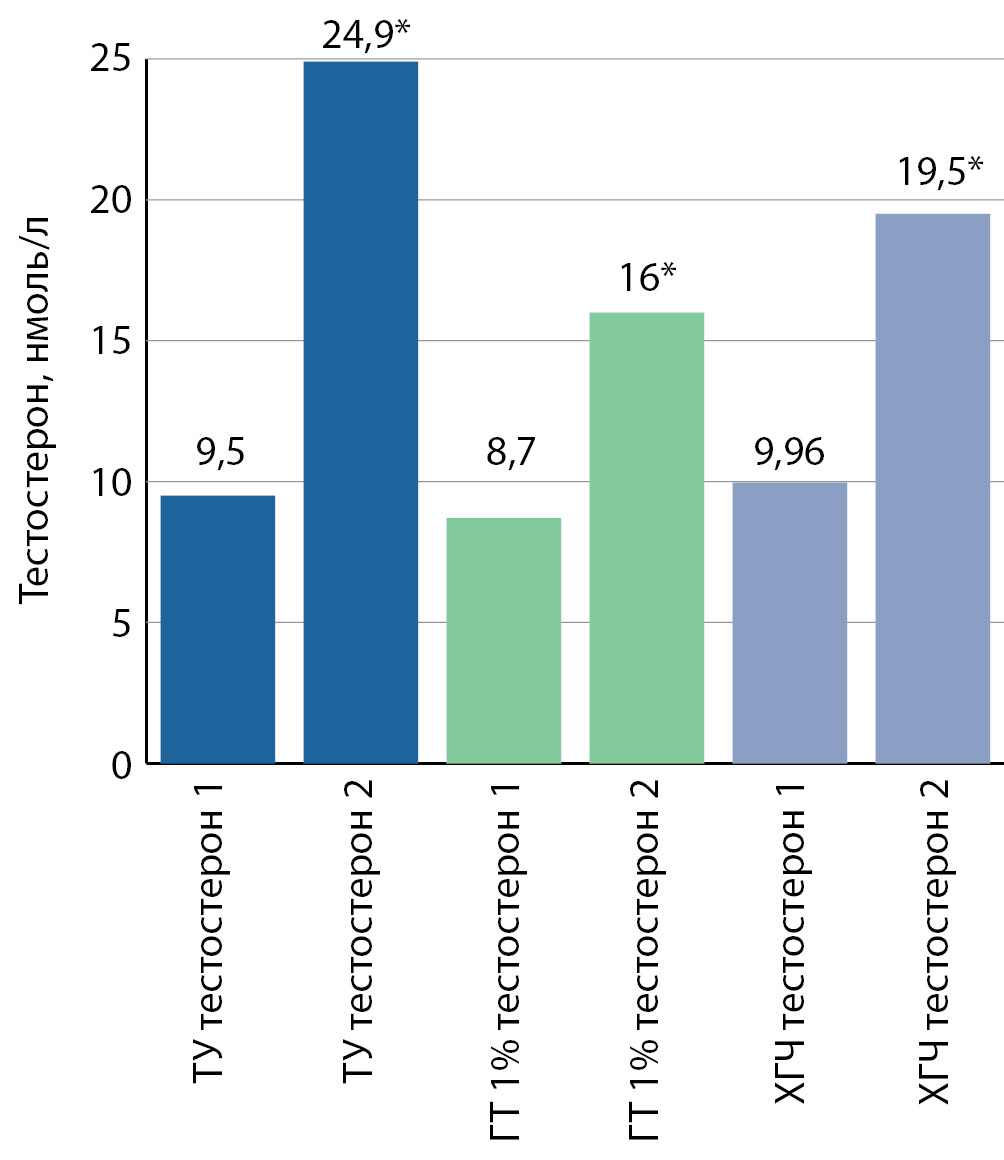
Materials and methods: For retrospective analysis, the medical records of patients with baseline testosterone deficiency and normal estradiol levels, who were prescribed TRT or hCG therapy, were selected. The patients were divided into 3 groups depending on the form of TRT and hCG therapy. The level of testosterone, estradiol, sex hormone binding globulin (SHBG), weight, OT, OB, BMI in each group was assessed 2 times — before the appointment of treatment and at different periods of treatment, for example, after 3–6–9 and 12 months. Most of the patients had a period of monitoring these parameters before the appointment of TRT or hCG therapy and after 6 months.
Results: The increase in the levels of total testosterone and estradiol against the background of TRT in the total sample was 109.6% and 111.3%, respectively. In each group, increases in total testosterone and estradiol levels were significant, p ≤ 0.001. The level of total testosterone to physiological values increased only in the 2-nd group — reaching the average-normal, recommended levels, from 8.7 ± 0.5 (2.5) to 16 ± 2 (10). The maximum rises in total testosterone, as well as estradiol, were noted in the 1st group, from 9.5 ± 0.72 nmol / L (3) to 24.9 ± 2.7 nmol / L (11.62)) and with 24.19 ± 2 (8.5) to 58.1 ± 4 (18.1), respectively. TRT, like hCG therapy, promotes an increase in the level of estradiol, which was demonstrated in all groups, and not only in group 1-st: in group 2-nd from 28.1 ± 2.3 (11.3) to 55 ± 4 (20) and in the 3-rd group from 27.1 ± 2.5 (10.5) to 55.8 ± 4.6 (19.6). On average for the entire sample, from 26.6 ± 1.32 (10.2) to 56.2 ± 2.5 (19). Weight loss on TRT was significant only in the 2-nd group, and in all parameters — weight, BMI, waist and hip circumference. In the 3-rd group, BMI, WC and OB values also slightly decreased. In the 1-st group, the total weight slightly increased, while the BMI did not change, as did the OB value, and the OT value decreased slightly.
Conclusion: TRT significantly increases the levels of total testosterone and estradiol, contributing to the normalization of testosterone levels, as in the 2-nd group, or the development of supraphysiological levels of total testosterone and hyperestrogenism, as in the 1st and 3-rd groups. Given that there is a strong belief that TRT leads to significant weight loss, our study confirmed this statement only in the 2-nd group.
Case Report
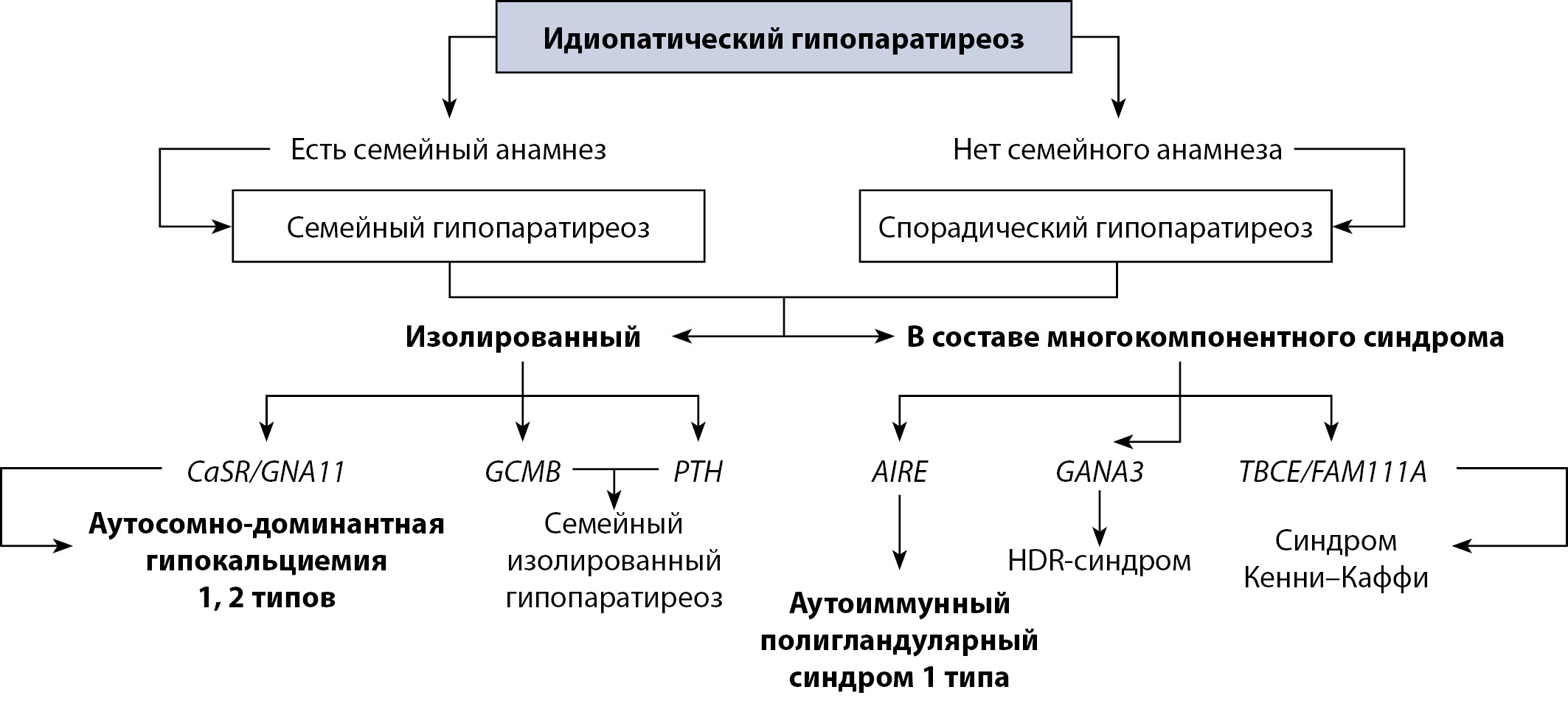
Idiopathic hypoparathyroidism is a rare endocrine disease diagnosed when all possible causes of hypoparathyroidism are excluded.
Data on the prevalence of idiopathic hypoparathyroidism is limited, there are several local studies in some countries. The variety and non-specificity of the hypoparathyroidism symptoms, similarity to other diseases (eg. epilepsy), causes the misdiagnosis and delay in pathogenetic therapy.
Idiopathic hypoparathyroidism is rare. Therefore, the absence of neck surgery in the anamnesis practically excludes hypoparathyroidism from the diagnostic search. Moreover, it is necessary to rule out all known causes of decreased PTH hypoparathyroidism to determine the form of non-surgical hypoparathyroidism.
We present a case series of idiopathic hypoparathyroidism, which demonstrates the difficulty in diagnosis, and the clinical features of the disease. The article covers also the problem of modern diagnostic approaches including the determination of the interferon-omega for patients with suspected autoimmune polyglandular syndrome type 1 as the most common cause of nonsurgical hypoparathyroidism.
Reviews
Obesity is a chronic disease characterized by excessive accumulation of adipose tissue. The prevalence of obesity and associated diseases has prompted researchers to expand the study of the biology of adipose tissue. New technologies have significantly expanded the understanding of adipogenesis mechanisms, various aspects of lipid and glucose metabolism, as well as the paracrine and endocrine functions of adipose tissue. Adipose tissue is a complex, heterogeneous endocrine organ. The existence of several shades of adipocytes demonstrates their morphological and functional heterogeneity. The main function of white adipose tissue is to store energy. Brown and white adipocytes perform a predominantly thermogenic function. Bone marrow (yellow) adipose tissue regulates the processes of bone remodeling and hematopoiesis. Pink adipocytes are formed during pregnancy and satisfy the energy needs of the offspring. The study of the biology of adipose tissue is crucial to understanding the pathophysiology of obesity and determining its molecular relationships with type 2 diabetes as well as cardiovascular and oncological diseases. The review presents current literature data on the origin, adipogenesis, and functional properties of adipose tissue depending on its cellular composition and localization. It outlines the nature of changes in adipose tissue in obesity and the clinical significance and therapeutic potential of various adipose tissue depots.
The prevalence of metabolic syndrome (MS) has a worldwide tendency to increase and depends on many components, which explains the complexity of diagnostics and approaches to the prevention and treatment of this pathology. Age, lifestyle, socioeconomic status, insulin resistance (IR), dyslipidemia, obesity and genetic predisposition are factors influencing the risk of developing and progression of MS. Features of the distribution and dysfunction of adipose tissue are important factors in the development of IR, with obesity, as well as the risk of the formation of cardiometabolic diseases and MS. Understanding of mechanisms is linked to advances in metabolic phenotyping. Metabolic phenotyping of obese persons is important for the development of important diseases in relation to the study of the pathophysiology of metabolic disorders, the possible concomitant disease and the search for innovative strategies for the prevention and treatment of MS. The understanding of MS mechanisms is associated with advances in metabolic phenotyping. Therefore, the relevance of further study of the pathophysiological mechanisms underlying various metabolic phenotypes of MS is one of the promising areas of modern scientific research. This review summarizes the current literature data on the prevalence of MS depending on gender, age, population, area of residence, education, level of physical activity, and many other parameters. Metabolic risks of MS development are detailed. Biological markers of MS are considered. The necessity of metabolic phenotyping of MS has been shown, which may have potential therapeutic value.
The widespread prevalence of non-alcoholic fatty liver disease (NAFLD) and type 2 diabetes mellitus (T2DM), as well as their combination, determines the need for a targeted analysis of this pathology in order to optimize approaches to the diagnosis and treatment of patients with NAFLD and T2DM. As components of the metabolic syndrome, these two diseases have largely similar mechanisms of development and progression, simultaneously increasing the risk of adverse outcomes in comorbid patients. Despite the common pathophysiological mechanisms, the question of the development of NAFLD and T2DM remains significant.
Upon conducting literature analysis, two main theories have been identified: alimentary and metabolic. According to the alimentary theory, the primary link in the pathogenesis is obesity and the associated excessive accumulation of free fatty acids and triglycerides in the liver, which subsequently leads to insulin resistance and the development of T2DM. In contrast, the metabolic theory considers diabetes-related insulin resistance as the first hit, which, regardless of obesity, creates preconditions for liver damage. In addition, the review focuses on the consideration of the new concept of Metabolic associated fatty liver disease (MAFLD) as a hepatic manifestation of the metabolic syndrome and considers the clinical phenotypes identified within this pathology. In conclusion, pathogenically based treatment goals in patients with NAFLD and T2DM are overcoming insulin resistance, correcting atherogenic dyslipidemia, and restoring the structures and functions of liver cells.
This review article presents data from the literature, which provide an idea of the relationship between metabolic disorders occurring against the background of obesity and endotoxinemia, as well as the effect of these conditions on the maintenance of low-grade inflammation in the body. A description of the hormonal and immune restructuring of white adipose tissue, the main routes of entry and metabolism of endotoxin is given. Particular attention is paid to the mechanisms of the mutual influence of obesity and endotoxinemia. Described by Yakovlev M.Yu. in 1988 «endotoxin aggression» and Cani P.D. et al. in 2007, «metabolic endotoxinemia», in our opinion, is one of the most important triggers for the development and progression of a whole spectrum of acute and chronic diseases. Based on the data of recent years, adipose tissue is an active endocrine organ capable of influencing both metabolic processes and the state of innate and acquired immune defense mechanisms. It has now been proven that high-calorie diets lead not only to an increase in overweight, but also to an increase in the level of endotoxin circulating in the blood. An in-depth study of the ability of obesity and endotoxinemia to potentiate the mutual pro-inflammatory effect can help both in understanding the pathogenesis of the main cardiovascular, autoimmune, allergic and infectious (including viral) diseases, and in the development of methods for non-pharmacological and drug correction of these conditions.
Some environmental chemicals capable of interfering with the endocrine regulation of energy metabolism and the structure of adipose tissue in the function of the reproductive, immune, cardiovascular and other systems are called endocrine disruptors or disruptors. According to the WHO definition, the term «endocrine disruptors» means: «Exogenous substances or mixtures thereof that alter the function (s) of the endocrine system and, as a result, cause adverse effects in the intact organism or in its offspring, or (sub) population.» This includes compounds to which humanity is exposed in daily life as a result of their use in pesticides, herbicides, industrial and household products, plastics, detergents, refractory impregnations and as ingredients in personal care products. This review will present the latest scientific data on various ERs, such as persistent organic pollutants (POPs): pesticides (mirex, chlordecane, endosulfan, hexachlorobenzene-HCB dichlorodiphenyltrichloroethane-DDT and its metabolites), industrial chemicals (bisphenol A, polybrominated ether -PBDE, polychlorinated biphenyls-PCB, nonylphenol, dioxins, perfluorooctanoic acid-PFOA, phthalates), pharmaceuticals (diethylstilbestrol-DES). ERs are regarded as compounds that cause obesity, since they have the ability to influence cellular processes associated with adipose tissue, initiating changes in lipid metabolism and adipogenesis. Analysis of scientific materials on this issue indicates that ERs are ubiquitous in the environment and have a detrimental effect on the health of animals and mankind. The scientific and practical interest in this article is based on the growing statistics of the development of such socially significant pathologies as obesity and related diseases, including diabetes mellitus, metabolic syndrome, cardiovascular diseases, menstrual irregularities, as well as cancer and infertility, for of which obesity is a risk factor.
The lymphatic system (LS) is one of the main integrative systems of the body, providing protective and transport functions. In recent years, interactions between LS and adipose tissue (AT) have been of particular interest. Lymphatic vessels play an important role in metabolic and regulatory functions of AT, acting as a collector of lipolysis products and adipokines. In its turn, hormones and adipocytokines that produced in adipocytes (including leptin, adiponectin, IL-6, TNF-α, etc.) affect the function of lymphatic endothelial cells and control the growth of lymphatic vessels. Cooperation between LS and AT becomes pathogenetically and clinically important in lymphedema and obesity. It is known that both primary and secondary lymphedema are characterized by increased fat accumulation which is associated with the severity of lymphostasis and inflammation. Similarly, in obesity, the drainage function of LS is impaired, which is accompanied by perilymphatic mononuclear infiltration in the AT. The development of these changes is facilitated by endocrine dysfunction of adipocytes and impaired production of adipocytokines. The increase in the production of inflammatory mediators and the disruption of the traffic of inflammatory cells causes a further deterioration in the outflow of interstitial fluid and exacerbates the inflammation of the AT, thereby forming a vicious circle. The role of lymphangiogenesis in AT remodeling in obesity needs further research. Another promising area of research is the study of the role of intestinal LS in the development of obesity and related disorders. It has been shown that the transport of chylomicrons from the intestine depends on the expression of a number of molecular mediators (VEGF-C, DLL-4, neuropilin-1, VEGFR-1, CD36/FAT, etc.)in the endotheliocytes of the intestinal lymphatic vessels, as well as the functioning of «push-button» and “zippering” junctions between endothelial cells. New approach to the treatment of obesity based on blockade of lymphatic chylomicrontransport has been experimentally substantiated. Further identification of the molecular mechanisms and signaling pathways that determine the remodeling of AT in lymphedema and obesity are likely to provide new approaches to the treatment of these diseases.
CLINICAL PRACTICE GUIDELINES
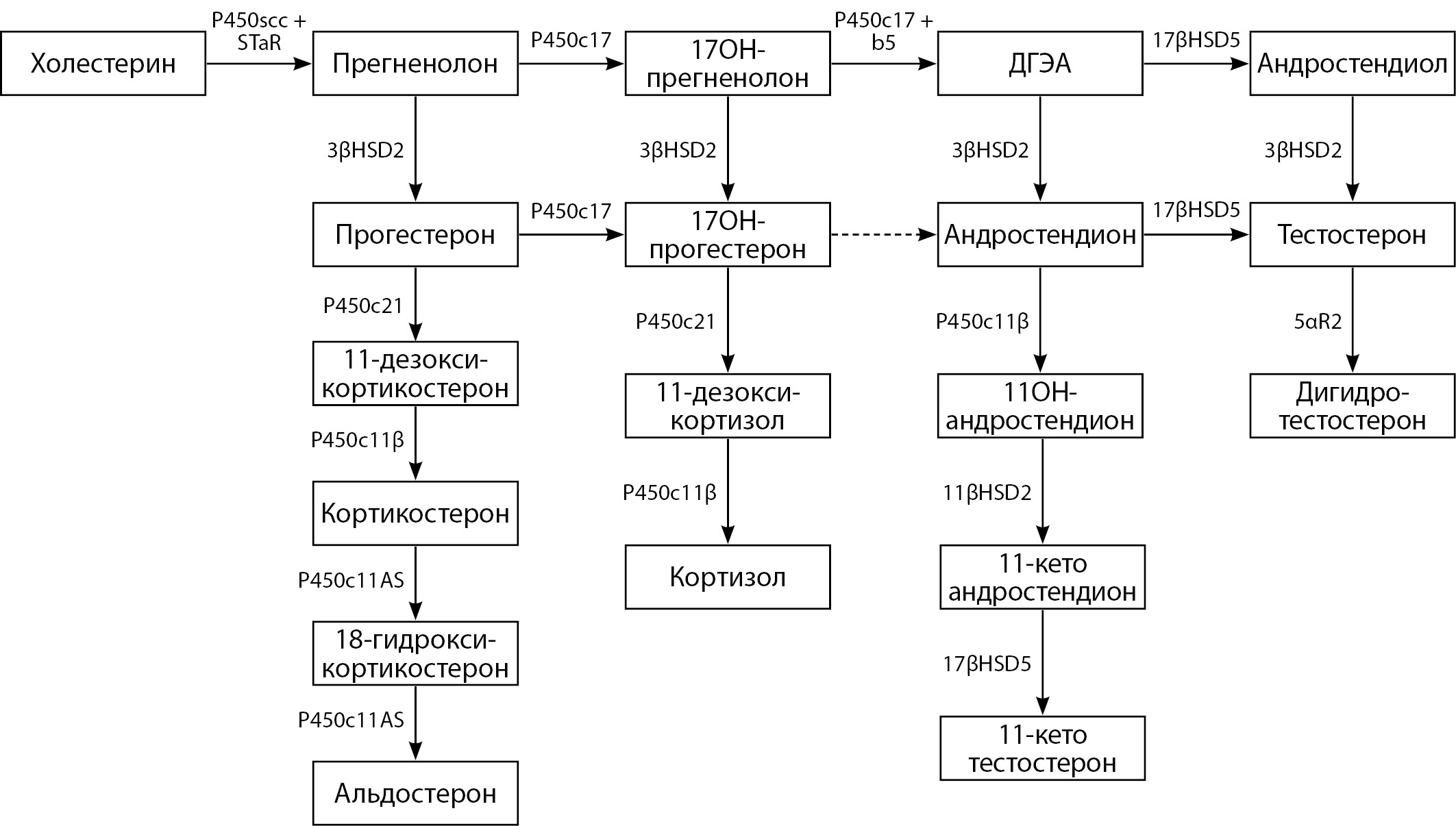
Congenital adrenal hyperplasia (CAH) is a group of autosomal recessive diseases characterized by a defect in one of the enzymes or transport proteins involved in the cortisol synthesis in the adrenal cortex. The most common form of CAH, which occurs in more than 90% of cases, is a 21-hydroxylase enzyme deficiency. The latter is subdivided into nonclassical and classic (salt-losing and virilizing) forms. The prevalence of classic forms of 21-hydroxylase deficiency ranges from 1: 14,000 to 1:18,000 live births worldwide. According to the data of neonatal screening in the Russian Federation, the prevalence of the disease in some regions ranges from 1: 5000 to 1: 12000, in the country as a whole - 1: 9638 live newborns. The non-classical form of CAH occurs more often - from 1: 500 to 1: 1000 among the general population. In second place is the hypertensive form of CAH - a deficiency of 11β-hydroxylase, which, according to the literature, occurs in about 1 per 100,000 newborns. These clinical guidelines were compiled by a professional community of narrow specialists, approved by the expert council of the Ministry of Health of the Russian Federation, and updated the previous version published in 2016. The clinical guidelines are based on systematic reviews, meta-analyses and original articles, and scientific work on this issue in the Russian Federation and other countries. The purpose of this document is to provide clinicians with the most up-to-date, evidence-based guidelines for the CAH diagnosis and treatment

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2306-5524 (Online)