ORIGINAL STUDIES
BACKGROUND: The steady annual increase in publications in the field of gut microbiota (GM) and insulin resistance indicates a growing recognition of the importance of this research topic.
AIM: To study the characteristics and relationships of GM metabolites and insulin resistance (IR) parameters in patients with arterial hypertension (AH) and to determine their role as indicators of AH progression.
MATERIALS AND METHODS: The comparative study included patients with stage II AGI, aged 25 to 65 years, receiving basic antihypertensive therapy. Patients in the study groups underwent laboratory testing of a biospecimen of blood and feces at the time of hospitalization. Analysis of gut microbiota parameters: the level of TMA, TMAO, short-chain fatty acids (SCFA), endotoxin; biochemical parameters by the lipid profile, fasting glucose, c-peptide, the concentration of C-reactive protein, gomocistein were determined; 24-hour blood pressure (BP) monitoring was performed by BPLaB device, Russia; study of the elastic properties of the vascular wall by sphygmography using the Vasera VS-1000 Series, PWV — pulse wave velocity (PWV). Statistical analysis was carried out using the IBM SPSS Statistics 21 application package.
RESULTS: The study included 161 patients who met the inclusion criteria, from which 3 main groups were formed: group 1 — persons without AH (n=45); group 2 — patients with stage I-III AH (n=53); group 3 — patients with stage I-III AH and abdominal obesity (AO) (n=63), matched by age, gender and therapy. Patients in group 3 differed significantly from patients in groups 1 and 2 in terms of BMI, WC, OB, and from group 1 in the values of office SBP, DBP (p < 0.001) and pulse wave velocity (PWV) (p=0.015). The levels of TMAO and endotoxin were also significantly higher in the 3rd group of patients compared to the 1st group. The total content of monocarboxylic acids: C2 — acetic acid, C3 — propionic acid, C4 — butyric acid is significantly higher in the 2nd and 3rd groups compared to the 1st group (p < 0.002, p < 0.004, respectively to the groups). In the groups with AH, the target level of TC and LDL-C indicators was significantly exceeded, and in the group of AH with AO — the maximum level of TG p=0.001, TyG index, interleukin 1β and hs-CRP (p=0.001). The dependence of PWV on SCLC2 and TyG C2 and SBP on TyG in the 3rd groups of patients was determined using the logistic regression method.
CONCLUSION: The close relationship between the TyG index and UA metabolites with PWV and SPB parameters may confirm the complex role of these factors in the development and progression of AH, especially in the presence of AO. The introduction of these diagnostic methods into clinical practice will facilitate the implementation of early preventive and therapeutic intervention strategies.
BACKGROUND: Identifying the nature of changes in body composition and the relationship with the clinical course of COPD is an urgent problem, since the data obtained can be used to assess the outcome and prognosis of the disease.
AIM: To establish the relationship between body composition and the characteristics of the clinical course of COPD.
MATERIALS AND METHODS: The study was conducted in the Clinics of the Siberian State Medical University, including the examination of invited patients from the City Clinical Hospital No. 3. This study is multicenter, interventional, two-sample, comparative. Patients with COPD and apparently healthy controls were included. All of them underwent anthropometry, questionnaires, bioimpedance measurements, spirometry and a test for the reversibility of bronchial obstruction.
RESULTS: 105 patients with COPD were conditionally divided into three groups according to BMI. The control group consisted of 40 people. The greatest number of patients with GOLD IV was observed in the group with normal body weight. Obese and overweight COPD patients have higher levels of lean body mass and visceral fat. Patients with GOLD stage I had the highest amounts of body fluid, mineral mass, visceral fat, and lean and lean body mas, and with stage GOLD IV had the lowest levels of muscle mass and adipose tissue. It was found that with a larger amount of adipose tissue, better indicators of external respiration function are observed. Visceral fat was positively correlated with CAT and CCQ scores.
CONCLUSION: Spirometry indicators in patients with COPD are related not only to muscle and fat tissue, but also to the amount of fluid in the body and mineral mass of the body. COPD patients with normal body weight had the least amount of adipose tissue and the worst FEV1. Patients with stage GOLD I had the highest amount of body fluid, mineral mass, visceral fat, as well as lean and lean body mass, while GOLD IV had the highest number of patients with a deficiency of lean body mass and excess adipose tissue. This highlights the importance of body composition assessment in the clinical management of patients with COPD.
BACKGROUND: The increase in the number of people with obesity is associated with an increase in the prevalence of cardiovascular diseases, justifying the search for new drugs to correct metabolic disorders.
AIM: To assess the metabolic effects of GABA derivatives (FPS and MFBA compositions) when used separately and in combination with sitagliptin in a model of carbohydrate metabolism disorder induced by alimentary obesity.
MATERIALS AND METHODS: The study was conducted on male rats with alimentary obesity. Following a six-month high-fat, high-calorie diet, seven groups were formed (n=8), including a positive control group (intact rats without obesity) and a negative control group, as well as five groups with comparable obesity severity. These groups received the studied compositions separately for 30 days: MFBA (20 mg/kg) and FPS (50 mg/kg), the reference drug sitagliptin (10 mg/kg), and combinations of MFBA+sitagliptin (20+10 mg/kg), FPS+sitagliptin (50+10 mg/kg). Upon completion of the treatment course, changes in body weight, visceral fat mass, lipid profile, and severity of carbohydrate disorders based on the oral glucose tolerance test and the insulin tolerance test were assessed. Levels of glucagon, insulin, and glucagon-like peptide-1 (GLP-1) were determined by enzyme-linked immunosorbent assay. The degree of liver damage was evaluated based on levels of liver transaminases (ALT and AST) and through morphological examination of structural changes.
RESULTS: It was established that the MFBA and FPS compositions, separately and in combination with sitagliptin, significantly reduced body weight and visceral fat mass, and enhanced the hypoglycemic action of sitagliptin (especially in combination with FPS). The separate and combined administration of MFBA and FPS with sitagliptin increased the levels of GLP-1 and insulin, improved glucose utilization, and increased insulin sensitivity, as well as normalized the lipid profile and levels of ALT, AST. Morphological examination revealed fewer foci of lymphoid infiltration and less pronounced fatty degeneration of the liver during treatment. The combination of FPS+sitagliptin showed the highest effectiveness.
CONCLUSION: GABA derivatives - MFBA and FPS, in monotherapy and more pronouncedly in combination with sitagliptin, reduced the severity of metabolic disorders associated with obesity. The anorexigenic effect noted for the cyclic GABA derivative (FPS) and the ability to improve carbohydrate and lipid metabolism are of interest for further studies.
BACKGROUND. Genomic imprinting disorders represent a distinct class of hereditary diseases caused by disruption of the monoallelic expression of imprinted genes. Several of them are closely associated with obesity and metabolic disturbances. Syndromes such as Prader–Willi, Angelman, Schaaf–Yang, Temple, and pseudohypoparathyroidism types 1a and 1b illustrate how dysregulation of imprinted gene expression can lead to energy imbalance, hyperphagia, reduced physical activity, and abnormal fat distribution. Currently, the proportion of early-onset and severe obesity cases caused by genetic factors is steadily increasing.
AIM. To study the clinical and genetic characteristics of syndromic forms of obesity in children.
MATERIALS AND METHODS. A retrospective non-comparative study. The study included 186 patients who were examined at the Endocrinology Research Center with suspected genetic forms of obesity in the period from October 2022 to May 2025.
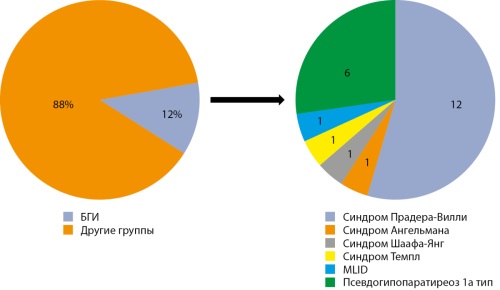
RESULTS. Genomic imprinting disorders were confirmed in 12% of patients (n=22), including: Prader–Willi syndrome (n=12), Angelman syndrome (n=1), Schaaf–Yang syndrome (n=1), Temple syndrome (n=1), multilocus imprinting disturbances (MLID) (n=1), and pseudohypoparathyroidism type 1a (n=6). At the time of examination: 13.6% (n=3) had overweight (BMI SDS 1.0–1.9 SD), 4.6% (n=1) had grade 1 obesity (BMI SDS 2.0–2.4 SD), 18.2% (n=4) had grade 3 obesity (BMI SDS 3.0–3.9 SD), and 40.9% (n=9) had morbid obesity (BMI SDS≥4.0 SD). Excessive weight gain during the first year of life was observed in 40.9% (n=9), and in 31.8% (n=7) starting from the second year of life. Clinical signs of hyperphagia were identified in 54.5% of cases (n=12). A positive family history of obesity was identified in 31.8% of cases (n=7). The median BMI SDS was 3.71 SD [1.8025; 4.2875]. Obesity- and overweight-related complications were observed in 13 out of 17 patients.
CONCLUSION. The study presents the genetic and clinical characteristics of genomic imprinting disorders within the structure of syndromic obesity in children in the Russian Federation.
AIM. To evaluate the effectiveness and safety of physical training of varying intensity in obese patients.
METHODS. A single-center open-label randomized trial of 37 obese patients. The patients were divided into three groups: group 1 — 15 patients 5–7 days a week for 60 minutes performed training walking at a speed reached at the level of 25–30% VO2peak, group 2 — 15 patients 5-7 days a week for 40 minutes performed training walking at a speed reached at the level of 60% VO2peak, group 3 — 7 Patients were trained to walk 3 times a week for 30 minutes at a speed reached at the level of 75-80% VO2peak. The dynamics of BMI, OT, and TFN were analyzed (based on the assessment of oxygen uptake at the peak of PH (VO2peak)).
RESULTS. The inclusion of patients in group 3 was prematurely discontinued due to poor tolerance of high-intensity interval training, therefore, a total of 7 patients were included in group 3. After 6 months of training, the most pronounced decrease in BMI and OT, as well as a greater increase in TFN, walking speed at the lactate threshold and the period of predominant fat absorption during physical training were recorded in group 1, whose patients trained at an intensity of 25–30% of VO2peak. According to the results of the analysis of the observation diaries, a high frequency of adverse events was revealed in the group of patients performing moderate and high intensity training.
CONCLUSIONS. 1. FT with an intensity of 75–80% VO2peak not well tolerated by obese patients and is less effective compared to FT with an intensity of 25–30% and 60% of VO2peak. 2. Aerobic workouts with an intensity of 25–30% VO2peak are the safest and most effective in obese patients.
BACKGROUND: Certain genes are involved in the regulation of nutrient and energy metabolism. The PPARGC1A and ACE genes, the products of which provide cellular energy metabolism, are actively studied not only in the development of relationships with the physical characteristics of individuals (sports results), but also in relation to pathological changes in the body, as a result of the appearance of metabolic products with altered physicochemical properties and parameters of functional activity, leading to various diseases (obesity, type 2 diabetes, insulin resistance, metabolic syndrome).
AIM: to conduct an associative search for genetic variants of the ACE (I/D) and PPARGC1A (G/A) genes with clinical phenotypes of obesity in children.
MATERIALS AND METHODS: The study included 177 children with obesity and 135 healthy children aged 5 to 18 years. The following were studied: nutritional status, lipid and carbohydrate metabolism parameters to conduct an associative search for genetic variants of the ACE (I/D) and PPARGC1A (G/A) genes with clinical phenotypes of obesity (OB).
Testing of polymorphic variants of the ACE (I/D), PPARGC1A (PGC-1) genes was performed by PCR and RFLP analysis.
RESULTS: In the sample of healthy children, the I/D and I/I genotype of the ACE gene and the A/A and G/A genotypes of the PPARGC1A gene are more common. In patients with obesity, the I/D genotype and the D allele of the ACE gene, and the G/A genotype of the PPARGC1A gene are more common.
The G/G genotype and the G allele of the PPARGC1A gene in obesity were associated with metabolic syndrome and hypertriglyceridemia
CONCLUSION: The I/D genotype of the ACE gene was more common in obese patients, but no associations of the genotype with metabolic risks were found. The G/G genotype of the PPARGC1A gene was more common in obese patients and was associated with the risk of developing metabolic disorders and hypertriglyceridemia.
The incidence of type 1 diabetes is increasing worldwide, especially among young patients. This trend is very unfavorable, since the risk of death of diabetic patients from cardiovascular and other concomitant diseases is five times higher than that of patients without a history of type 1 diabetes. The main causes of premature mortality are micro- and macrovascular complications, aggravated by concomitant diseases, one of which is arterial hypertension. The risk of complications such as acute cerebral circulatory disorders, myocardial infarction, limb amputation, heart failure and sudden cardiac death increases with increasing duration and severity of hypertension, especially with its uncontrolled course. Patients with type 1 diabetes who are under inpatient or outpatient supervision and treatment, for the most part, do not control blood pressure, or are guided by data from home/office blood pressure measurements. In our opinion, it is worth paying special attention to screening diagnostics, early detection, as well as profiles of increased blood pressure in patients with type 1 diabetes, as this will allow us to consider the possibility of initiating antihypertensive treatment or optimizing therapeutic approaches to the management of this group of patients, and is also key to reducing the risk of adverse outcomes of this disease.
REVIEWS
The problem of obesity and metabolic syndrome is becoming increasingly global in the modern world. The social and environmental factors that play a role in the development of these conditions are not yet fully understood, but there is already accumulating evidence that the development of obesity and metabolic syndrome is promoted by unfavorable conditions in early life, such as maternal diseases during pregnancy and lactation, the use of various chemical and medicinal agents, low birth weight of the fetus, and unfavorable dietary patterns and quality of nutrition. All these factors have their impact on the gastrointestinal tract, particularly leading to an imbalance of the intestinal microflora. Evidence is accumulating that the gut microbiome of obese people is structurally and functionally different from the gut microflora of healthy people. The identification of a strong correlation between these parameters may offer prospects for the prevention of metabolic syndrome and all associated conditions by maintaining the health of the gut microflora. The aim of this article is to highlight the data from animal and human studies that confirm the presence of pathophysiological mechanisms of the influence of the intestinal microflora on the development of obesity and the associated metabolic syndrome, and to search for opportunities to prevent these conditions through the addition of pre- and probiotics to food.
Metabolic syndrome-related diseases account for two-thirds of non-communicable disease deaths, most of which may begin early in life. The pro-inflammatory environment observed in obese MS patients may contribute to immune dysregulation in COVID-19 patients, including suboptimal immune responses, hyperinflammation, microvascular dysfunction, and thrombosis. Exercise may be a key intervention to reduce inflammation in obese COVID-19 patients as it may reduce adipocyte number and size, as well as inflammatory response and cytokine expression associated with excess adipose tissue-mediated immune dysregulation. Given the increasing number of people with metabolic syndrome and the significance of this pathology in the context of the consequences of the COVID-19 pandemic, as well as the importance of physical activity in the treatment, rehabilitation and prevention of cardiometabolic risk factors, it is necessary to consider the main aspects of the pathogenesis of MS, the features of rehabilitation strategies in patients with metabolic syndrome and obesity with the consequences of previous NVI. The aim of the review was to search, summarize and discuss the available literature data on the development and pathogenesis of metabolic syndrome in the long-term post-COVID period, as well as systematize the available methods of cardiac rehabilitation in this category of people.
MATERIALS AND METHODS: The search and selection of literary sources was carried out in the system of published research in scientific databases cyberleninka.ru, elibrary.ru, link.springer.com, frontiersin.org, pubmed.ncbi.nlm.nih.gov, Web of Science, Google Scholar and others.
Cardiovascular diseases (CVDs) have long been the leading cause of mortality and morbidity worldwide. It has been demonstrated that disturbances in calcium-phosphate metabolism, particularly primary hyperparathyroidism (PHPT), may further contribute to their development and progression. Despite the established association between PHPT and CVD, many aspects of this relationship remain insufficiently explored. The state of the cardiovascular system plays a decisive role in assessing patient mortality; however, there are currently no clear predictors of CVD development in PHPT. At present, cardiovascular pathology is not listed among the absolute indications for surgical treatment of parathyroid gland disorders. Nevertheless, given the high prevalence of hypertension and other CVDs, the updated national guidelines on PHPT now include a mandatory cardiology consultation for all patients to assess cardiovascular health and prepare for potential surgery. The aim of this article is to review recent research on the impact of PHPT on the cardiovascular system, analyse the underlying pathogenic mechanisms, and discuss diagnostic and treatment strategies for this patient group. A comprehensive assessment of cardiovascular changes — with an emphasis on their pathogenetic basis — is essential for improving both the quality and longevity of life in the population.
In the world, more than 2 billion people are overweight, which makes up 30-39% of the world’s population. Against the background of existing obesity, comorbid pathology is progressing in patients.
The article provides information on the pathogenetic basis of obesity. The features of functioning and hormonal activity of adipocytes are described. The mechanisms of the effect of hormones and metabolically active substances produced by adipocytes on the human body, the development of comorbid pathology are considered. all of them have been studied in detail.
Based on the analysis, it can be assumed that unexplored metabolites secreted by adipose tissue may play a key role in the regulation of metabolism, inflammatory processes and even in the development of various diseases, including obesity. The low effectiveness of obesity treatment, despite financial costs exceeding 2 trillion US dollars annually, actualizes the revision of existing approaches, the development of new treatment methods and medicines based on a deeper understanding of the pathogenetic foundations of obesity.
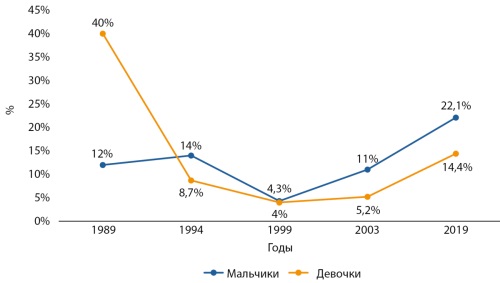
This review analyzes the prevalence of childhood and adolescent obesity in the Russian Federation. Data from various regional studies are provided. In some regions, long-term obesity dynamics were studied. The history of studying the epidemiology of obesity in Russia spans more than thirty years. According to the data obtained, the prevalence of childhood obesity throughout the country remains high and continues to increase. In all regions where long-term trends were assessed, the prevalence of obesity has increased (maximum 15.8% in the Tyumen Region). Among children, obesity is recorded among boys more often (maximum 38.3% in St. Petersburg) compared to girls (maximum 37.4% in St. Petersburg).
CASE REPORT
Thyroid hormones are involved in the activation of glycogenolysis and mitochondrial oxidative phosphorylation. Kocher–Debré–Semelaigne Syndrome, also known as hypothyroid myopathy, is characterized by reduced glycogenolytic activity, leading to glycogen deposition in muscles. These reserves begin to deplete as euthyroidism is achieved.
Primarily, patients complain of muscle weakness, mainly in the proximal muscle groups, stiffness, myalgia, and cramps. A distinctive feature of hypothyroid myopathies is the reversibility of clinical manifestations and a significant improvement in well-being with medical compensation of the disease. However, the absence of a pronounced clinical picture of hypothyroidism, combined with its rare occurrence, complicates early diagnosis and often requires differential diagnosis with other types of myopathies. This article presents a clinical case of a combination of genetically determined myopathy with extrapyramidal symptoms, associated with a mutation in the MICU1 gene, and hypothyroid myopathy associated with congenital hypothyroidism in a patient from a consanguineous marriage.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2306-5524 (Online)