ORIGINAL STUDIES
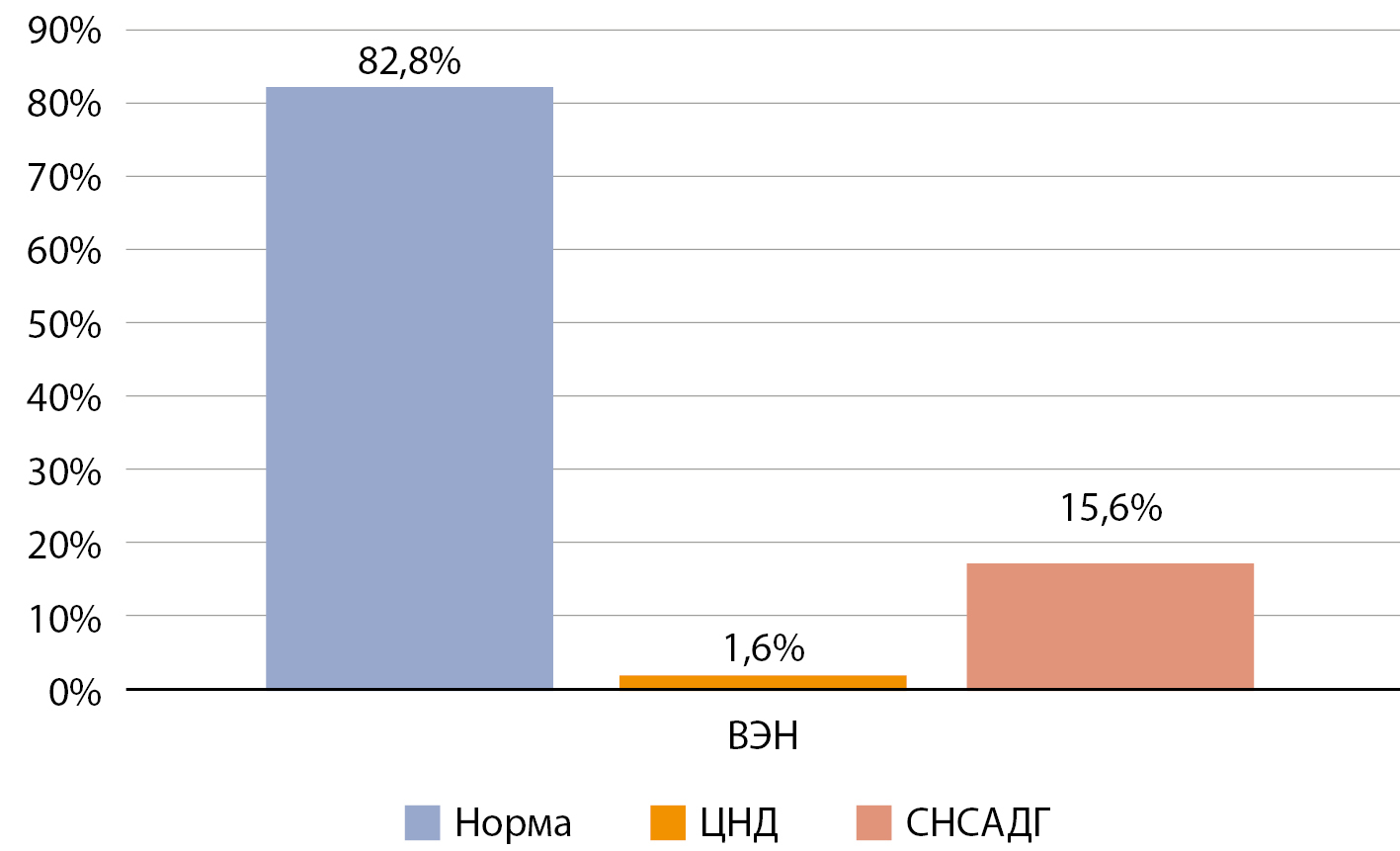
BACKGROUND: To date, the causes and predisposing factors for the development of water-electrolyte disturbances after transsphenoidal surgery for hypothalamic-pituitary masses are poorly understood. Neuropeptides such as apelin, copeptin, and brain natriuretic peptide, discovered in recent decades, have been shown in many studies to have a significant effect on the regulation of water-electrolyte metabolism and make them potential hormonal markers of severe postoperative electrolyte complications.
AIM: to study the features of secretion of hypothalamic neuropeptides during normal water and salt metabolism in the perioperative period and in the presence of water and electrolyte metabolism disorders.
MATERIALS AND METHODS: Patients above 18 years of age who were scheduled to undergo transnasal adenomectomy for underlying disease were included in the study. Patient recruitment was conducted from March 2021 to March 2022. All patients were monitored initially and further in the postoperative period of transnasal adenomectomy for the presence of water-electrolyte disturbances by blood sodium determination, as well as determination of apelin-12, copeptin, brain natriuretic peptide, and oxytocin levels in the first 12–24 hours, then on days 2–3, 4–5 and 6–7 postoperatively. Patients also filled in a diary of well-being and water balance.
RESULTS: It has been established that such a water-electrolyte complication as hyponatremia aggravates the postoperative period of transnasal adenomectomy in up to 15% of cases.Our study revealed no significant changes in the levels of apelin and brain natriuretic peptide or their correlation with the level of sodium in patients in both groups, as well as the relationship between neuropeptides. The most interesting effects on water-electrolyte metabolism are demonstrated by the neuropeptides oxytocin and copeptin, the secretion of which has the character of inadequately elevated levels with loss of inverse negative correlation with blood sodium concentration.
CONCLUSION: Our study revealed a high incidence of hyponatremia after transnasal adenomectomy — about 15% of cases, in the genesis of which hypothalamic neuropeptides copeptin and oxytocin seem to play a significant role. Oxytocin has the potential to be a hormonal marker of this severe complication.
BACKGROUND: Psoriasis is characterized by a high frequency of comorbid metabolic disorders, including obesity and type 2 diabetes mellitus. There are limited data on the efficacy of glucagon-like peptide-1 receptor agonist for the treatment of metabolic disorders in patients with psoriasis.
AIM: Analysis of the effectiveness of liraglutide in the complex therapy of patients with psoriasis in combination with metabolic disorders.
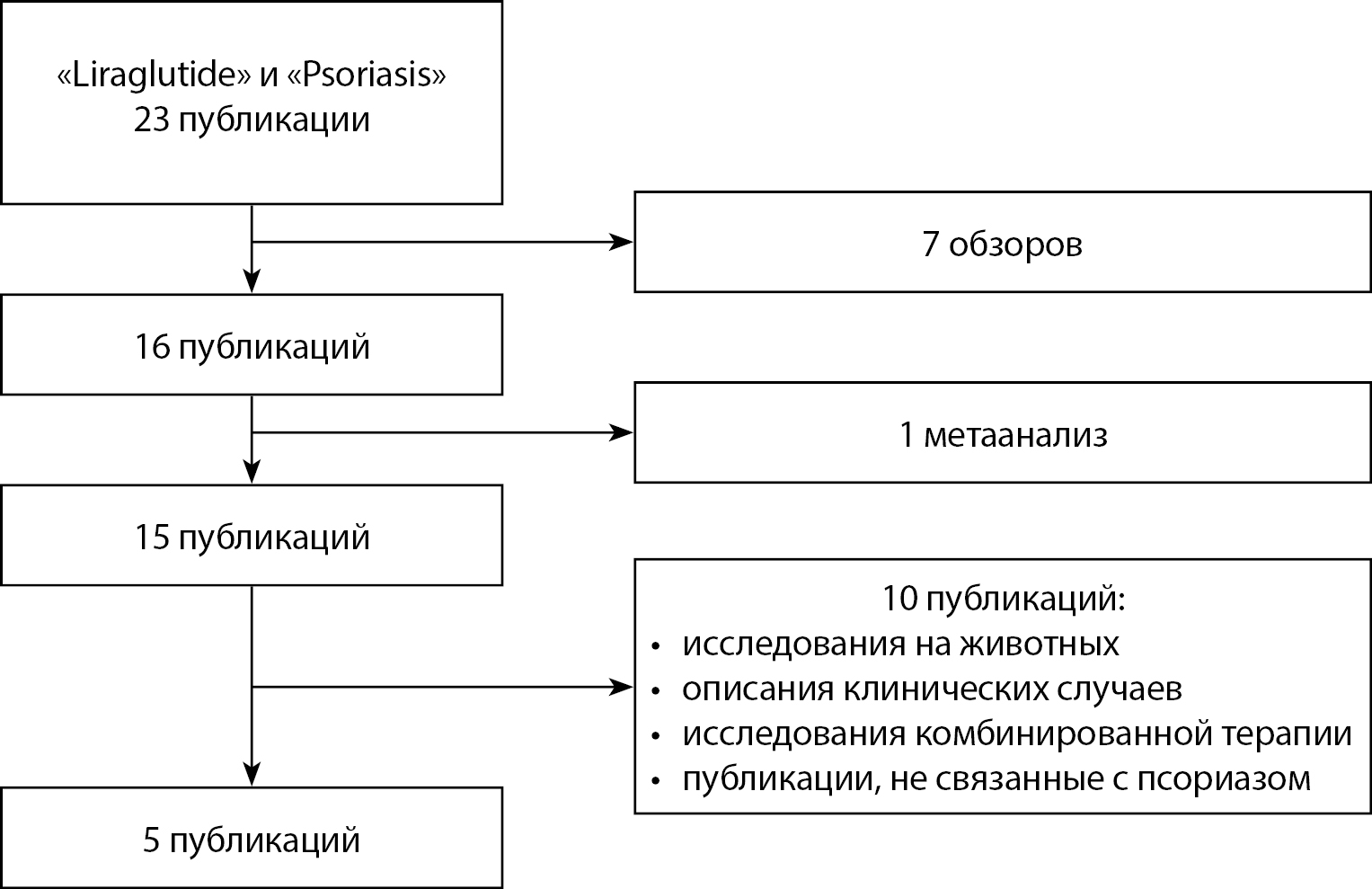
MATERIALS AND METHODS: The PubMed database was searched for studies using the keywords "psoriasis" and "liraglutide". 23 publications were found, the final analysis included 5 studies with a total sample size of 52 patients with psoriasis combined with metabolic disorders (type 2 diabetes mellitus and obesity). The effect of liraglutide on the prevalence and severity of psoriasis was assessed by the dynamics of the lesion area and psoriasis severity index (PASI), quality of life according to the DLQI questionnaire and the level of fasting plasma glucose, glycated hemoglobin, and body mass index. The results are presented as the weighted mean difference (WMD) and 95% confidence interval (CI).
RESULTS: The duration of liraglutide therapy ranged from 8 to 16 weeks. The liraglutide dose was titrated from 0.6 mg/day to 3.0 mg/day. Significant dynamics of the WMD indices PASI (-6.95 [95% CI -11.59; -2.32]) and DLQI (-6.95 [95% CI -11.59; -2.32]), as well as the body mass index (-2.97 [95% CI -3.58; -2.37]) were demonstrated during liraglutide therapy. No significant difference in glucose and glycated hemoglobin levels was found.
CONCLUSION: The results of the meta-analysis demonstrate that the use of liraglutide in combination therapy for psoriasis helps to reduce BMI, the prevalence and severity of psoriasis, and improve the quality of life of patients.
OBSERVATION. In the modern world, where overweight and obesity are becoming more and more widespread, a particularly alarming factor is the appearance of morbid forms among young children (up to 7 years old), which is the most atypical phenomenon and is of particular interest in the search for the causes of this pathology. According to the published data, about 7% of cases of severe pediatric obesity are associated with various genetic disorders. At the same time, the prevalence of monogenic and syndromal obesity in the Russian population remains unknown.
OBJECTIVE. To study the clinical features and genetic characteristics of patients with obesity occurring in early childhood.
MATERIALS AND METHODS. We examined 115 patients (49 girls (42.6% of cases, 95% CI [33.4; 52.1]), 66 boys (57.4% of cases, 95% CI [47.8; 66.5]) with obesity (SDS BMI >3.0) and the disease debut at an early age (up to 7 years). All patients underwent a comprehensive examination. Genetic study included full-exome sequencing by NGS (next-generation sequencing) or genetic analysis by methyl-sensitive multiplex ligase-dependent probe amplification (MS-MLPA) (in case anamnestic, phenotypic, clinical data suggestive of genomic imprinting diseases are identified).
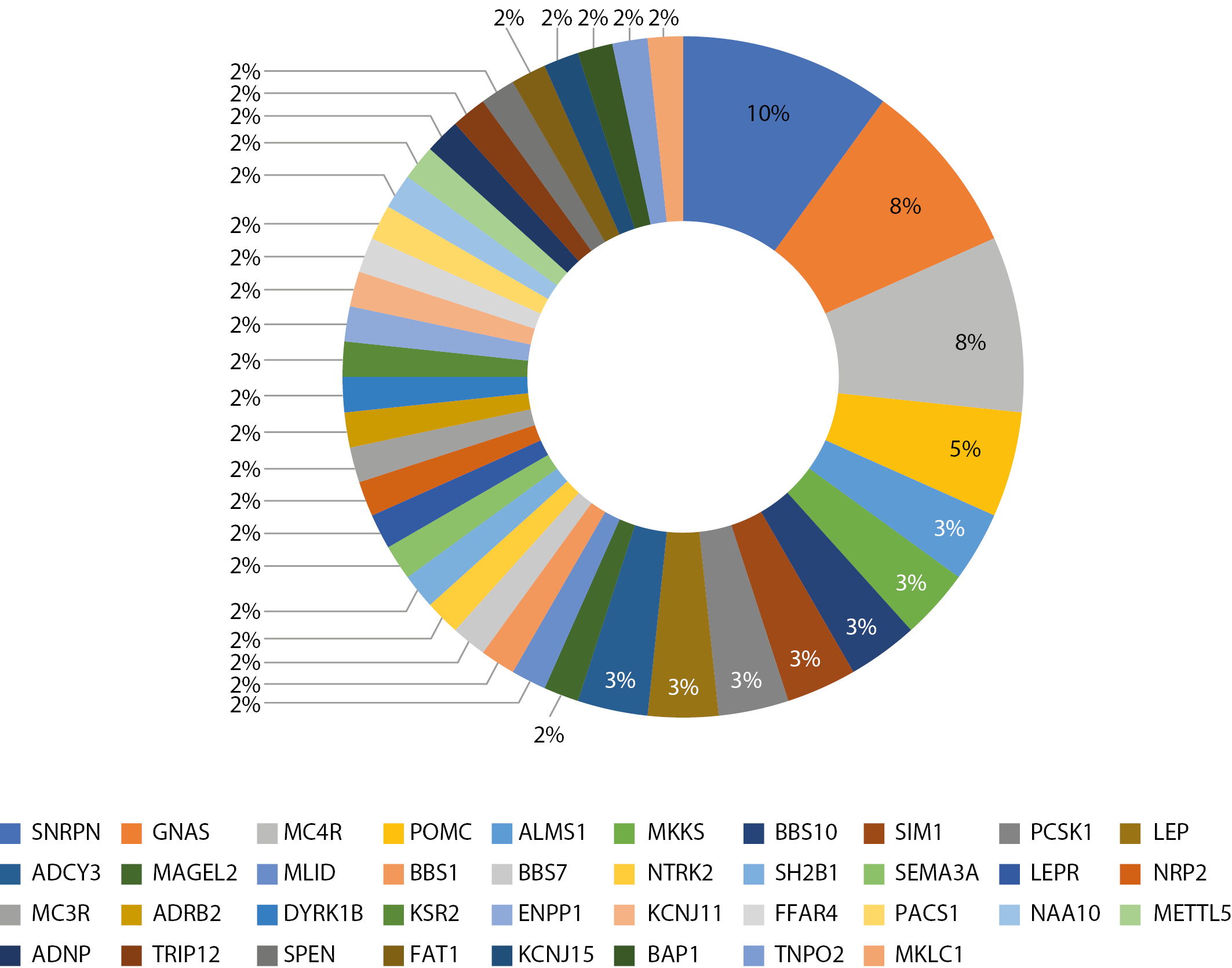
RESULTS. In our study, 48.7% of children showed nucleotide sequence changes in the following genes: SNRPN, GNAS, MC4R, POMC, ALMS1, MKKS, BBS10, SIM1, PCSK1, LEP, ADCY3, MAGEL2, BBS1, BBS7, NTRK2, SH2B1, SEMA3A, LEPR, NRP2, MC3R, ADRB2, DYRK1B, KSR2, ENPP1, KCNJ11, FFAR4, PACS1, NAA10, METTL5, ADNP, TRIP12, SPEN, FAT1, KCNJ15, BAP1, TNPO2, MKLC1, SNRPN, GNAS. As per the results of the genetic study, the patients divided into 2 groups: group 1 — “genetic obesity”, group 2 — “obesity with unidentified cause”. The median age of patients at the time of examination was 8.2 years [5.5; 13.6], and the SDS of BMI was 4.0 [3.6; 4.4]. Patients in both groups were comparable in age, SDS of BMI, and SDS of height. In obese patients with an unspecified cause, an aggravated hereditary history of obesity was statistically significantly more common than in patients with genetic disorders (p<0.001). Polyphagia in patients with genetic disorders occurred in more than 79% of cases, whereas in patients with “simple” obesity this symptom was completely absent (p<0.001). The incidence of metabolic complications of obesity, such as carbohydrate metabolism disorders, insulin resistance, nonalcoholic fatty liver disease, and arterial hypertension did not differ statistically significantly between patients in both groups.
CONCLUSIONS. The high percentage of detected genetic alterations in our cohort might be explained by the strict criteria for inclusion of patients in the study, which emphasizes the relevance of this work. Further study of the pathogenetic mechanisms of obesity will contribute to the development of targeted therapy, which will allow the development of a personalized approach to the treatment and prevention of this disease.
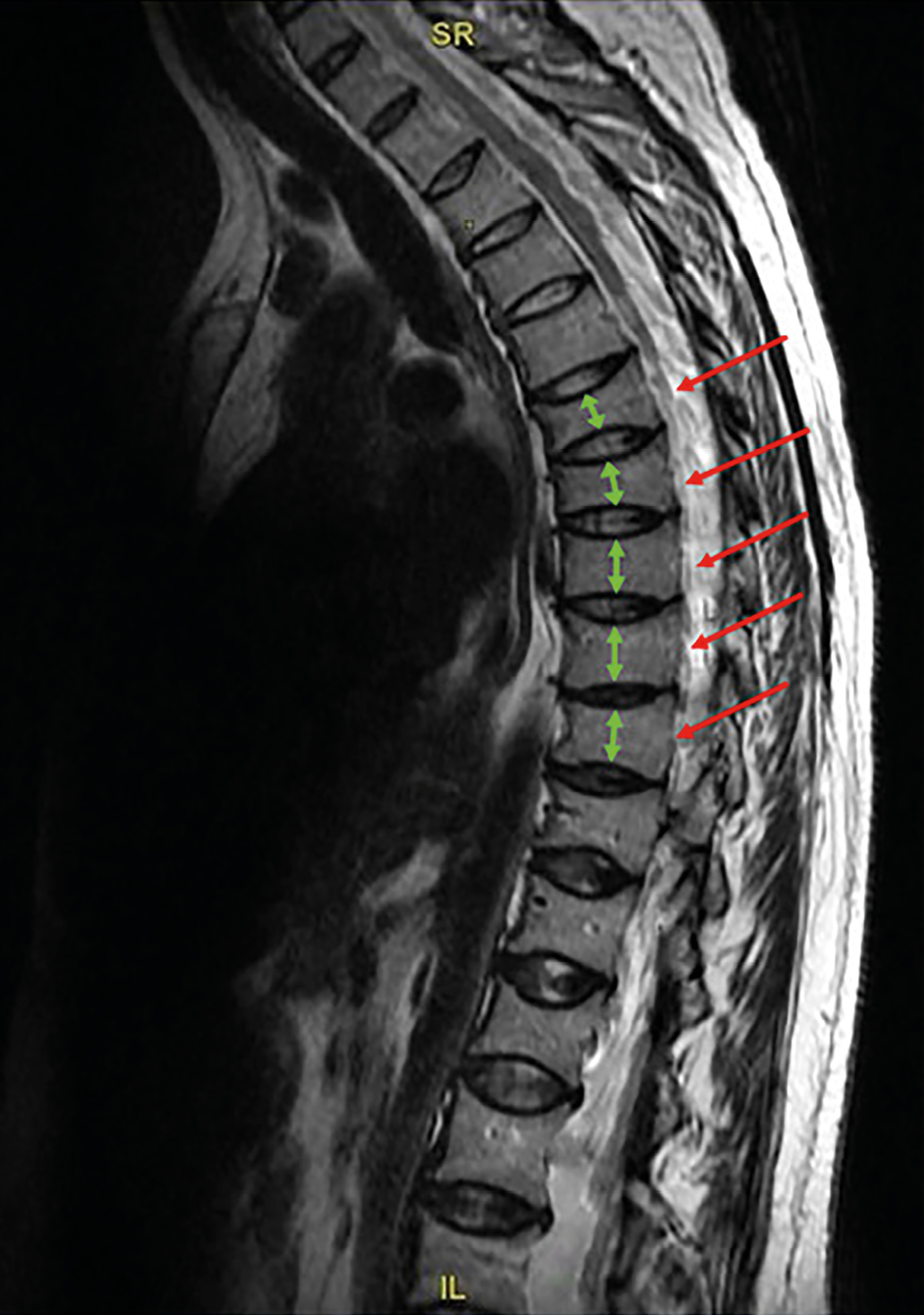
BACKGROUND: Acromegaly is a severe neuroendocrine disorder caused by growth hormone hypersecretion, leading to various organ-system complications. In acromegaly, radiographic signs of osteoarthritis (OA) involving multiple joints develop even before the diagnosis of acromegaly is established and continue to progress over time, despite biochemical remission.
AIM: To identify the features of spinal, thoracic cage, and shoulder girdle joint involvement in patients with acromegaly.
MATERIALS AND METHODS: A single-center, observational, cross-sectional, retrospective comparative study. The study included patients with acromegaly; the sample was formed using a consecutive sampling method. Recruitment period: October 2022 — November 2024. A comparison of the features of the spinal, thoracic cage, and shoulder girdle joints was conducted between patients with acromegaly and a control group.
RESULTS: The study included 98 patients with acromegaly, including 55 women (56.1%) and 43 men (43.9%). The mean age at diagnosis was 36 [31; 45] years, and at the time of examination, 39.5 [32; 46] years. The control group included 12 men (48%) and 13 women (52%). The median age was 45 [39; 54] years.
In patients with acromegaly, radiographic signs of costovertebral OA were associated with older age and were more frequent in 35 patients with a median age of 44 [39; 54] years (p=0.001), with a cutoff point of ≥39 years. OA of the acromioclavicular joints was more frequent in males (p=0.006). When comparing the two groups, costovertebral OA was more frequent in patients with acromegaly (p=0.001).
CONCLUSION: Costovertebral OA can be considered a specific musculoskeletal disorder in patients with acromegaly, while spondyloarthrosis, OA of the sternocostal, shoulder, and acromioclavicular joints are not. The results of our study demonstrate the need for a comprehensive assessment of MSK pathology in patients with acromegaly. The obtained data can serve as a basis for improving rehabilitation algorithms and differential diagnosis of comorbidities in this cohort of patients.
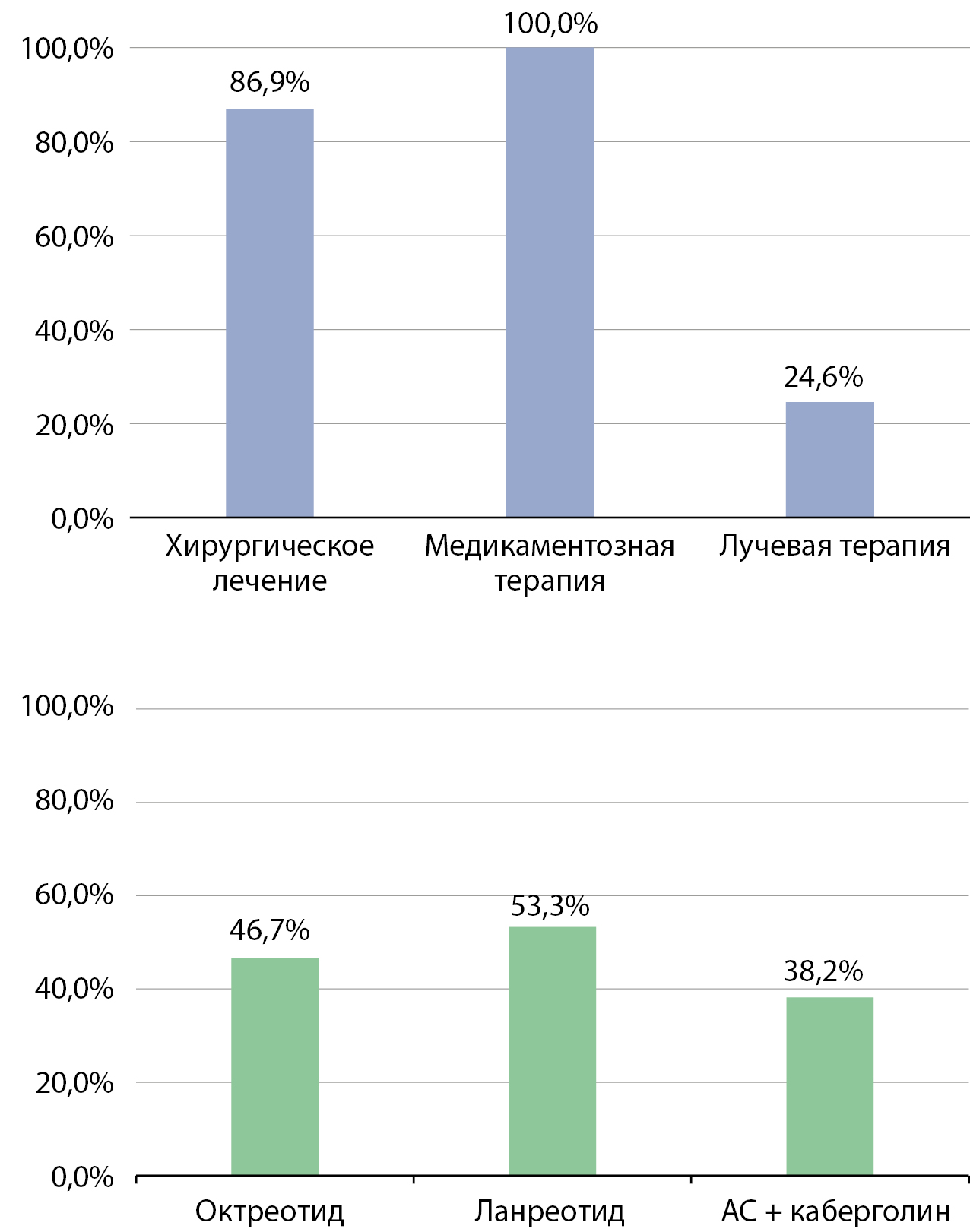
BACKGROUND: Acromegaly is a chronic neuroendocrine disorder, the prognosis of which depends on timely and adequate treatment. A high percentage of non-radical surgical treatment and the problem of resistance to first-line drug therapy necessitate the timely inclusion of second-line drugs.
AIM: To evaluate the efficacy and safety of pegvisomant (PEG) therapy in patients with unsatisfactory acromegaly control.
MATERIALS AND METHODS: The characteristics and treatment outcomes of 185 patients with acromegaly who did not achieve biochemical remission with somatostatin analogs were analyzed. These patients received PEG therapy at three medical centers in Moscow, Russia, between 2019 and 2024. During treatment, dynamic monitoring of insulin-like growth factor 1 (IGF-1) levels, carbohydrate metabolism indicators, liver transaminases, and contrast-enhanced magnetic resonance imaging (MRI) of the brain were performed.
RESULTS: PEG treatment resulted in sustained biochemical remission of acromegaly in 70.8% of patients. The average daily PEG dose was 15 mg. A direct relationship was established between the drug dose and the initial IGF-1 level, body mass index (BMI), and glycated hemoglobin level. The use of the drug was not associated with significant changes in pituitary adenoma size or the development of serious adverse events.
CONCLUSION: Timely inclusion of a second-line drug (PEG) in the treatment regimen of patients who did not achieve control with high-dose monotherapy with somatostatin analogs allows for achieving sustained biochemical control of acromegaly with minimal side effects.
REVIEWS
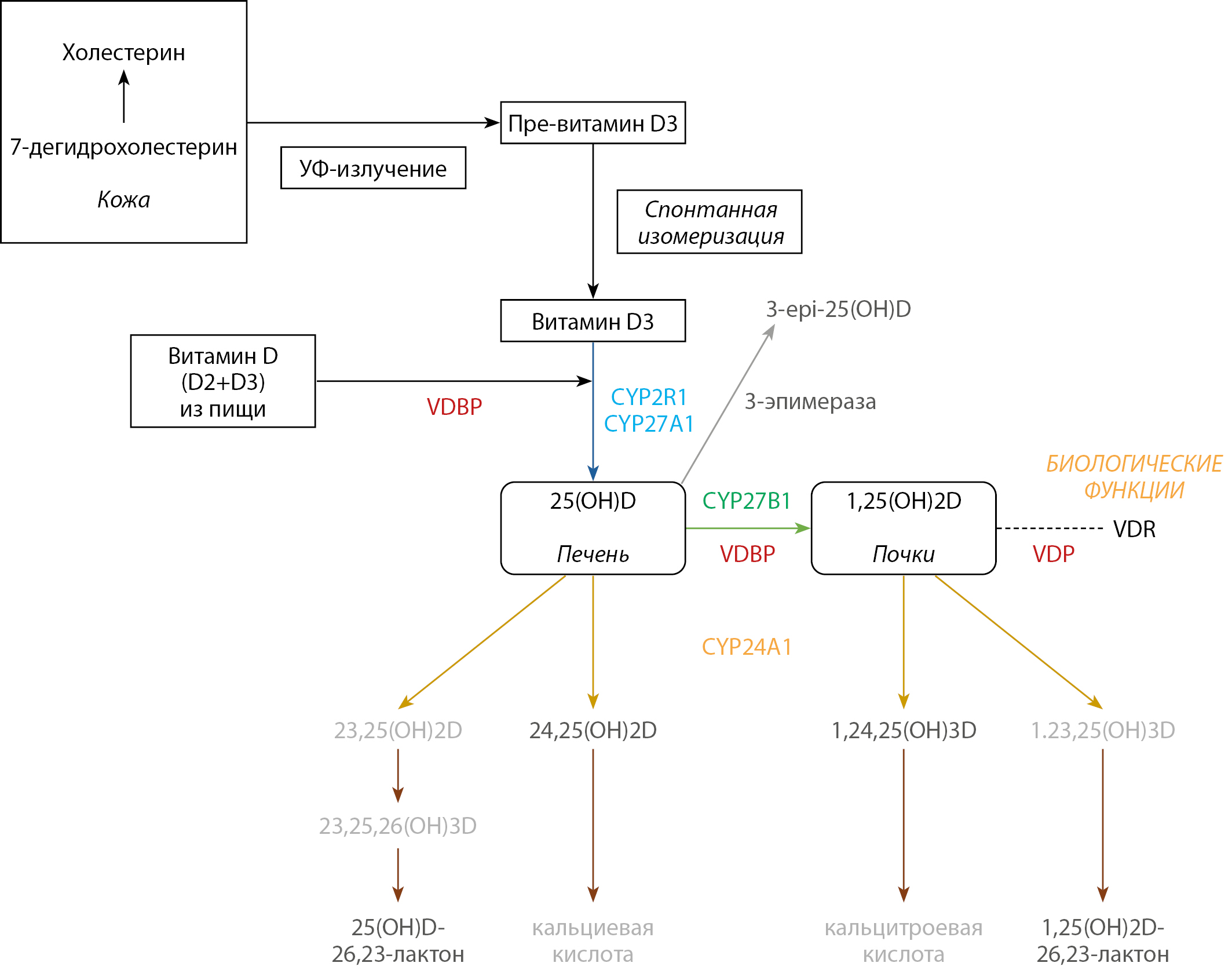
Vitamin D plays an important role in the regulation of the «mother-placenta-fetus» system, participating in ensuring normal growth and development of the fetus, reducing the risks of hypocalcemia, muscle cramps, respiratory infections in childhood. To date, the existence of more than 50 metabolites of vitamin D has been established, of which the most studied are total 25-hydroxyvitamin D (25 (OH) D) and 1,25-dihydroxyvitamin D (1,25 (OH) 2D), which is due, first of all, to their importance for the endocrine regulation of calcium-phosphorus metabolism. The level of 25 (OH) D in the blood is an optimal, but not perfect marker of vitamin D status, and does not reflect the numerous effects of its metabolites. Taking into account the special metabolic adaptation of a woman’s body during gestation, the analysis of quantitative changes in various vitamin D metabolites is of particular relevance. This review summarizes the available data on the characteristics of vitamin D metabolism outside gestation and during pregnancy.
In today’s world, characterized by the growing prevalence of endocrine diseases and the complexity of their diagnosis and treatment, AI offers unique opportunities to improve medical care. In the article, we analyze how AI algorithms help detect and classify pathological changes in ultrasound, MRI, CT providing endocrinologists with additional tools for fast and accurate diagnosis. In addition, we are considering the use of AI for big data analysis, including electronic medical records (EHRs), which allows us to develop predictive models and personalize treatment. Special attention is paid to the role of AI in monitoring patients with chronic endocrine diseases, including continuous monitoring of blood glucose levels in diabetes mellitus
This article will be useful for endocrinologists, researchers, students and anyone interested in the use of artificial intelligence in modern medicine.
According to epidemiological studies, the number of patients with type 1 diabetes mellitus (DM1) in the Russian Federation is 277.1 thousand people. The number of patients continues to grow, as well as the prevalence and mortality rates, especially the negative trend is the average age of those who died from DM1, in particular for the female sex for the period from 2010 to 2022 this indicator decreased from 62.1 to 56.0 years. Glycation of structural molecules of organs and tissues leads to their dysfunction and subsequent disability of the patient. Despite the development of pharmacological industry and widespread availability of insulin preparations, not all patients reach target values of glycated hemoglobin. The development of secondary disorders mediated by insulin deficiency and impaired glycemia, such as dyslipidemia, low-intensity inflammation, metabolic endotoxinemia, and oxidative stress leads to vascular channel wall damage, significantly increasing cardiovascular risk in patients with DM1. Taking into account the whole spectrum of pathogenetic disorders in patients with DM1, a promising direction is the search for additional ways of regulation, including the use of biologically active compounds contained in plant materials, and in particular polyphenols. Literature data confirm the anti-inflammatory, antioxidant and hypoglycemic effects of polyphenols. Given the wide availability of polyphenols in the diet, their multifactorial impact on metabolic pathways, these compounds are a promising tool to influence the pathogenesis of various pathologies, including DM1. In view of the above, this review focuses on the influence of plant polyphenols, in particular grape polyphenols, on the pathogenesis of DM1, and possible ways of using polyphenol-rich foods/drugs to reduce risks in patients with DM1. By analyzing the MedLine (PubMed) databases, a search was conducted using the keywords, «diabetes type 1», «polyphenols», «inflammation» and «dyslipidemia» and a search of the eLibrary library using the keywords, «diabetes type 1», «polyphenols», «inflammation» and «dyslipidemia». Most of the scientific articles presented in this literature review were published in the last 5 years. The data presented in this review suggest that grape polyphenols are a potential agent that, in combination with mainstream disease therapy, can influence the underlying pathogenetic mechanisms of DM1, leading to improved glycemic control, achievement of lipid profile targets, and reduction of oxidative stress. Further study of polyphenols contained in grapes and grapes products will make it possible to create an effective and, most importantly, safe therapeutic agent for the reduction of cardiorespiratory stress.
CASE REPORTS
Diabetes insipidus (DI) is an orphan disease clinically characterized by profound thirst and the excretion of large volumes of dilute urine. Nephrogenic diabetes insipidus (NDI) is characterized by resistance to the action of antidiuretic hormone (ADH). Hereditary NDI is associated with mutations in the vasopressin receptor gene, AVPR2, in 90% of cases; less frequently, defects in the aquaporin-2 gene (AQP2) are observed. This clinical case presents a novel mutation in the AVPR2 gene (hemizygous mutation c.587T>C, p.Phe196Ser), which has not been previously documented in the literature, identified in a 29-year-old male. The patient reports significant thirst and polyuria since early childhood. The diagnosis of nephrogenic diabetes insipidus (NDI) was confirmed at three years of age against a backdrop of severe polyuria-polydipsia syndrome, aided by a water deprivation test. No increase in urine osmolality was observed following the administration of desmopressin. Magnetic resonance imaging (MRI) of the brain did not reveal any structural anomalies. Genetic analysis conducted at the age of 29 identified a rare mutation resulting in the substitution of phenylalanine (Phe) with serine (Ser) at position 196 of the receptor protein (p.Phe196Ser). The patient was advised to take a thiazide diuretic alongside potassium supplements, which led to a reduction in thirst and a decrease in urine output. However, after two weeks of treatment, symptomatic hypokalemia developed, necessitating the discontinuation of hydrochlorothiazide. Following this cessation, potassium levels stabilized, but NDI symptoms recurred. Therapy with non-steroidal anti-inflammatory drugs (NSAIDs) did not yield significant clinical effects. A decision was made to resume hydrochlorothiazide at a lower dose, in combination with potassium supplements and a potassium-sparing diuretic. The patient is under ongoing observation. This clinical case emphasizes the importance of an interdisciplinary approach in the differential diagnosis and treatment of diabetes insipidus, aimed at preventing complications and improving the quality of life for patients with polydipsia-polyuria syndrome.
Pregnancy and lactation are accompanied by physiological changes in mineral-bone metabolism, aimed at meeting the needs of the developing fetus and newborn while maintaining the mother’s health. Due to these changes, particular attention should be paid to the consumption of calcium-rich foods, adequate intake of vitamin D, moderate physical activity, and sufficient sunlight exposure. Bone pathologies observed in the later stages of gestation often manifest with similar clinical symptoms, despite significant pathogenetic differences, which increases the risk of diagnostic and therapeutic errors. This article presents a clinical case of osteomalacia that likely developed long before pregnancy but was diagnosed only after prolonged treatment with anti-osteoporotic and anabolic therapy. The paper discusses the challenges of differential diagnosis between osteomalacia and pregnancy and lactation associated osteoporosis, emphasizing the importance of an interdisciplinary approach and the need to raise awareness among specialists, particularly radiologists, for the timely identification of the disease and the prescription of pathogenetically grounded treatment.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2306-5524 (Online)