ORIGINAL STUDIES
AIM: to identify the features of immune reactions in practically healthy individuals in response to short-term cold exposure, depending on the level of total cholesterol in the blood.
MATERIALS AND METHODS: On the basis of the Laboratory of Ecological Immunology of the Institute of Physiology of Natural Adaptations of the Federal Research Center for Integrated Arctic Studies named after Academician N.P. Laverov of the Ural Branch of the Russian Academy of Sciences, 108 practically healthy women living in Arkhangelsk aged 21 to 50 years were examined. Blood was taken from the ulnar vein on an empty stomach in the morning before and immediately after general cooling for 5 minutes at a temperature of -25 °C. The complex of immunological studies included the study of venous blood hemograms: the number of platelets, erythrocytes, leukocytes, total hemoglobin in the blood, leukograms, phagocytic activity of neutrophils and blood monocytes, determination of cytokines IL-1β, IL-6, TNF-α. The study of the lipid profile included the determination of total cholesterol, glucose, triglycerides, phospholipids.
RESULTS: In the Q1 group, no cases of hemoglobin deficiency were recorded, while in the Q4 group, hemoglobin deficiency was recorded in 14.29% of the surveyed, and after a short–term general cooling — in 21.43%. The total number of platelets, as well as the thrombocrit index in the Q4 group was significantly higher (259.07×10^3 cells/µl and 0.27%, respectively). The Q4 group had higher average monocyte levels in the leukocytogram (0.40±0.10×10^9 cl/l and 6.26±1.43% compared with 0.24±0.06×10^9 cl/l and 4.46±1.40%, p<0.05). It was revealed that persons from the Q1 group with higher background levels of CD4+, CD71+ lymphocytes are sensitive to short-term general cooling and whose CD4+, CD8+, CD25+, CD71+, CD56+ cells decrease by 1.3–1.6 times after visiting the cold chamber. The cytokine profile in the Q4 group was characterized by higher levels of IL-1β (7.13 pg/ml) and TNF-α (14.3 pg/ml). After short-term cold stress, a twofold increase in TNF-α was observed in the Q1 group from 6.77 to 13.33 pg/ml, and in the Q4 group a sharp decrease in IL-1β from 7.13 to 3.44 pg/ml.
CONCLUSION: The immunological background in the Q4 group of subjects with cholesterol levels close to the upper limit of the norm is in a more tense state, due to reactions from monocytes and lymphocytes of peripheral blood, higher levels of proinflammatory cytokines. The response to short-term general cold exposure is more pronounced in individuals of the Q1 group with minimal cholesterol levels. In 14.29% of people with cholesterol levels close to the upper limit of the norm, peripheral blood hemoglobin deficiency was recorded, and after short–term cold exposure — in 21.34%.
BACKGROUND: Cytokines secrete all cells when there is a threat of damage to it. Leptin, having all the properties of a cytokine, produces fat cells. It was of interest to identify the ratio of leptin concentrations and cytokines activating preventive inflammatory reactions in the blood of practically healthy Northerners with hyperlipoproteidemia.
AIM: To identify the ratio of concentrations of leptin and IL-1ß, TNF-α, IL-6 and IL-10 in the blood of practically healthy Northerners with hyperlipoproteidemia.
MATERIAL AND METHODS: A survey of 286 practically healthy people aged 35-55 years living in the Arkhangelsk region was conducted. The body mass index in persons of the first group (n=211) was in the range of 19.5-26.8 kg/m2 and corresponded to the norm; and 75 people of the second group (body mass index 31-40 kg/m2). Concentrations of leptin, interleukin-1β (IL-1β), tumor necrosis factor alpha (TNF-α), interleukin-6 (IL-6) and interleukin-10 (IL-10) were determined in the blood by enzyme immunoassay on an automatic Evolis enzyme immunoassay analyzer from Bio-Rad (Germanytotal cholesterol (OH), apolipoprotein A-1 (ApoA-1), apolipoprotein B (ApoV), high-density lipoproteins (HDL), low-density lipoproteins (LDL), very low-density lipoproteins (VLDL), oxidized low-density lipoproteins (LDL), triglycerides (TG), phospholipids (FL) on the biochemical analyzer «Stat fax 1904 Plus» of the company «Awareness Technology, Inc.» USA.
RESULTS: Fasting hyperlipoproteidemia in practically healthy people is associated with an increase in the concentration of leptin in the blood within the physiological content. The closest relationship between an increase in leptin levels and concentrations of proinflammatory cytokines IL-1ß, TNF-α and IL-6 was established (r=0.68, 0.74 and 0.83, respectively; p<0.001). The severity of the reaction of proinflammatory cytokines is regulated by a parallel increase in the secretion of anti-inflammatory IL-10 (r=0.62; p<0.001).
CONCLUSION: It should be recognized that the stimulation of leptin secretion is provided by the influence of more intense signals initiating a cytokine reaction. In order to ensure the secretion of leptin, compared with that of proinflammatory cytokines, the influence of more pronounced signals associated with an increased need for metabolic energy is required. Higher concentrations of leptin were found with a low plasma content of HDL, ApoA-1 ligands and ApoB; The opinion is substantiated that leptin in physiological concentrations regulates the use of the depot of the energy substrate of adipose tissue by increasing its secretion with a low content of HDL in plasma, ligands of lipid transport forms.
BACKGROUND: Obesity is a progressive health and economic problem of modern society. Endocrine-metabolic changes in childhood and adolescence have an impact on cognitive status, which is accompanied by changes in the perfusion of gray and white matter of the brain, as well as its architectonics.
AIM: Verification of fatty acid (FA) levels in relation to cognitive function and brain neuroimaging data in adolescents with obesity.
MATERIALS AND METHODS: The study is a single-center observational one-stage comparative. 60 teenagers aged 10–16 years were selected to participate. The main study group was formed of 34 adolescents with obesity (SDS BMI ≥+2.0), 26 subjects with normal weight made up the control group. The calculation of SDS BMI was performed on the WHO «Anthroplus» calculator. To obtain anthropometric data, a vertical height meter MSK — 233, scales and a soft centimeter tape were used. The levels of free fatty acids in the blood serum were determined by chromatomass spectrometry on the Agilent 7000B detector. For neurocognitive testing, the Montreal Cognitive Function Assessment Scale and the Ray test were used. Contrast-free perfusion magnetic resonance imaging of the brain was performed on a Signa Creator “E” MR tomograph by GE Healthcare, 1.5 Tl, China, by Arterial Spin Labeling. For MR tractography, the GE Sygna Creaton 1.5 Tesla apparatus was used using the method of diffusion imaging with high angular resolution HARDI (High Angular Resolution Diffusion Imaging). Statistical processing of the obtained results was carried out using IBM SPSS Statistics software.
RESULTS: According to the results of a comparative analysis, adolescents with obesity were distinguished by an increased content of free LC and a decrease in cognitive functions (p <0.05). A lot of statistically significant correlations of different groups of LC with changes in cognitive characteristics, cerebral blood flow and pathways were also obtained.
CONCLUSION: The results obtained confirm the significant role of free fatty acids in the pathogenesis of obesity and indicate the effect of lipotoxicity on morphological changes in the structures of the central nervous system, which can lead to the formation of cognitive disorders.
BACKGROUND: Obesity is a pathology that highly contributes to the development of type 2 diabetes mellitus and cardiovascular diseases. Meanwhile, different obesity phenotypes have varying levels of risk, and the indication of early predictors that can help determine the likelihood of developing cardiometabolic disorders is an important task. Since obesity is characterized by excessive energy intake, hormones involved in energy homeostasis (leptin and other adipokines, ghrelin, incretins) can be considered as serious candidates for the role of such predictors. The profile of changes in their level in the post-nutrition status testifies in favor of the development of resistance not only to insulin, but also to leptin, and to ghrelin, and, possibly, to incretins.
AIM: This study aims to investigate the relationship between the dynamics of the level of hormones involved in energy homeostasis in a sample with a standard carbohydrate breakfast and metabolic health.
MATERIALS AND METHODS: Metabolic parameters (including НОМА-IR and НОМА-B, lipid profile, glucose level, blood pressure) were assessed in 90 obese patients (BMI 37.31±4.83 kg/m2). Additionally, biomarkers such as adiponectin, CRP were measured. Levels of leptin, ghrelin, GLP1 and GIP were assessed before and 60 minutes after a standard carbohydrate breakfast. These hormone levels were classified depending on the nature of the changes, considering the physiological dynamics described in the literature in healthy people or not. Patients were divided into groups of metabolically healthy and metabolically unhealthy obesity, first using the most commonly known criteria (Meigs et al.), then based on the criteria discussed in the literature for perfectly healthy obesity, in which there are no metabolic disorders.
RESULTS: The analysis revealed that patients without metabolic disorders had a ghrelin level profile similar to that in healthy people without obesity, while patients with at least one of the manifestations of the metabolic syndrome showed evidence of ghrelin resistance (the level of ghrelin on an empty stomach was reduced, and after food it was not adequately reduced). Adiponectin levels were normal in metabolically healthy patients. Incretin levels showed unidirectional changes in obesity, regardless of metabolic status. The level of CRP did not differ between the groups. The glycemic level was significantly lower in metabolically healthy patients (the group was characterized by normal insulin levels and had a lower degree of insulin resistance).
CONCLUSION: The data obtained allow us to consider ghrelin resistance as an early and rather sensitive indicator of the development of metabolic disorders in obesity.
BACKGROUND: Recent clinical descriptions have shown that in adult patients, the cause of nondiabetic hypoglycemia (NDH) may be various genetically determined disorders of glucose metabolism or insulin synthesis/bioavailability. In this connection, in adult patients with NDH of unclear genesis, it is important to conduct a genetic study in order to search for mutations in genes associated with congenital disorders of glucose metabolism (CDGM).
AIM: To evaluate the effectiveness of genetic testing to exclude CDGM in adult patients with idiopathic NDH.
MATERIALS AND METHODS: Based on the analysis of the literature, a targeted panel has been developed, including 30 genes, mutations in which are associated with the following groups of diseases: 1) congenital hyperinsulinism (KCNJ11, ABCC8, GLUD1, HADH, UCP2, HNF4A, HNF1A, GCK, INSR, SLC16A1); 2) glycogen storage diseases (AGL); 3) other carbohydrate metabolism disorders (ALDOB, FBP1); 4) glycosylation defects (PMM2, ALG3, PGM1, MPI); 4) defects in fatty acid oxidation (ACADM, ETFA, ETFB, ETFDH, FLAD1, SLC25A32, SLC52A1, SLC52A2, SLC52A3); 5) disorders of ketone body metabolism (CPT1A, CPT2, HMGCL); 6) mitochondrial disorders (DLD). Twenty nine patients (n=29: with idiopathic NDH n=17 and with insulinoma n=12) aged 19 to 66 years underwent a genetic study using this custom panel.
RESULTS: As a result of the examination 12 genetic variants (all heterozygous) were identified in 8 patients with idiopathic NDH (47%, 95% CI (23%; 72%)), at that two mutations were detected in three patients: in the genes AGL and HMGCL; ACADM and FLAD1, respectively; and one patient had three mutations: one mutation in the ETFA gene and two mutations in the ABCC8 gene. Frequencies of genetic variants: AGL — 18%, 95% CI (4%; 43%), ETFA — 12% (1%; 36%), HMGCL — 6% (0%; 29%), ALDOB — 6% (0%; 29%), CPT1A — 6% (0%; 29%), ABCC8 — 6% (0%; 29%), ACADM — 6% (0%; 29%), FLAD1 — 6% (0%; 29%). 5 genetic variants (all heterozygous) were identified in 5 patients with insulinoma (42%, 95% ДИ (15%; 72%)). Frequencies of genetic variants: ABCC8 — 17%, 95% CI (2%; 48%), HNF1A — 8% (0%; 38%), ETFDH — 8% (0%; 38%), MPI — 8% (0%; 38%). We did not include benign variants in this analysis. At the same time, clinically significant variants were identified only in one patient from the group with idiopathic NDH (6%, 95% CI (0%; 29%)) in the ABCC8 gene and in one patient from the group with insulinoma (8%, 95% CI (0%; 38%)) in the same gene congenital hyperinsulinism (CHI).
CONCLUSION: A panel of 30 genes has been developed, variants of which are associated with a CDGM. The results of our study confirm the possibility of detecting CDGM in adulthood, in particular CHI, and indicate the need for genetic testing, primarily in patients with idiopathic NDH.
AIM: The purpose of this study was to analyze the characteristics of management, diagnosis and treatment of patients with vitamin D deficiency/ by endocrinologists in the regions of Russian Federation using a sociological survey.
MATERIALS AND METHODS: A cross-sectional sociological uncontrolled study was carried out. To implement this work, we used an online questionnaire “Questioning doctors on vitamin D” specially developed on the basis of the Google forms platform. The study was conducted in January 2021.
All the data obtained were entered into an electronic database in MS Excel. Statistical processing was performed using the IBM SPSS Statistics 25 software.
RESULTS: The survey involved 707 physicians from 86 regions of the Russian Federation. Our study revealed that not all doctors strictly adhere to clinical recommendations in patient management. Issues identified include unjustifiably widespread ordering of 25(OH)D blood tests (58.5%), lack of consideration for individual patient characteristics and clinical situations in dose selection (99.2%) and prescription of active metabolite or analogs of vitamin D to correct low 25(OH)D levels in blood (14.7%). Furthermore, recommendations for improving clinical guidelines focused on the lack of illustrative material (21.1%), expanding patient information sections (20.7%), and insufficient coverage of issues arising in clinical practice (14.6%). Our study also highlighted limited capabilities of laboratory diagnostics for assessing vitamin D status in patients in Russia. The survey revealed that only 9.2% of respondents have the ability to measure 1,25(OH)2D concentrations, and only 1.4% can order tests for 24,25(OH)2D. About 8.3% of participants did not specify which tests for assessing vitamin D status are available for prescription. Technical enhancement of laboratories and the inclusion of all recommended laboratory study requirements in the compulsory health insurance system could address this.
Regarding vitamin D toxicity, 25% of surveyed doctors encountered it. Main causes included self-administration of elevated doses of cholecalciferol by patients (62%) or prescribed by physicians (40%), the use of active metabolites or analogs of vitamin D (21%), incorrect dosing of cholecalciferol preparations as indicated by the manufacturer (18%), and defects in CYP24A1 (13%). Rare causes included granulomatous and lymphoproliferative diseases (11.5%).
CONCLUSION: The current clinical guidelines of the Russian Association of Endocrinologists for «Vitamin D Deficiency in Adults» are generally effective and widely used by clinicians. However, they do not entirely meet the needs of specialists and require refinement in terms of improving structure and clarity of presentation, expanding illustrative material, and justifying the frequency of laboratory diagnostics. Cases of vitamin D toxicity observed in clinical practice were predominantly associated with incorrect administration of vitamin D supplements. The identified high frequency of vitamin D toxicity in real clinical practice necessitates additional attention to this issue during the update of clinical recommendations.
BACKGROUND. Due to its role as a risk factor for the emergence of metabolic illnesses including type 2 diabetes, cardiovascular disease, and certain cancers with pandemic evolution, obesity is a serious public health concern. Diabetes mellitus type 2 (T2DM) poses a major risk to human health. The byproducts of the breakdown of cholesterol are bile acids, which are crucial for preserving cholesterol homeostasis. Research indicates that bile acids might control insulin sensitivity, energy metabolism, and glucose tolerance. Farnesoid X receptors (FXRs) are crucial for controlling bile acid production and hepatic glucose metabolism. The ligand for FXR The semisynthetic derivative of chenodeoxycholic acid, a bile acid, is obeticholic acid (OCA). Research indicates that bile acids may be a viable therapeutic target for type 2 diabetes (T2DM) given that therapy with oleic acid (OCA) enhanced insulin sensitivity and decreased indicators of liver inflammation and fibrosis in individuals with T2DM and nonalcoholic steatohepatitis (NASH).
AIM. To assess Obeticholic acid’s effectiveness in obese individuals with prediabetes.
MATERIALS AND METHODS. Over the course of three months, we performed a randomized single blind placebo controlled trial on eighty-two overweight and obese patients with prediabetes in the outpatient clinic at Ain Shams University Hospital. Through block randomization, patients were split into two groups (Group A received daily oral tablets containing 5 mg of obeticholic acid, while Group B received non-sweet capsules as a placebo). Three follow-up visits were conducted to ensure adherence and monitor for any emergence of side effects.
RESULTS. 82 patients of matched age and sex criteria who underwent block randomization into 2 equal groups, group (A) representing cases and group (B) the placebo controlled group, with 3 months’ regular follow up showed at end of treatment statistically significant difference in weight being lower in group (A) with p-value 0.004 with decreased parameters of glycemic profile (Fasting insulin, FPG, HOMA_IR, 2h PP, HbA1c) in group (A) with p-value <0.001 except 2hpp which p-value is 0.006. Also ALT was much decreased in group (A) with p-value <0.001. Lipid profile didn’t show significant difference between 2 groups except for TGs which deceased in follow up in group (A) with p-value <0. 001. Additionally, it should be highlighted that there was no statistically significant difference between the control group’s baseline and post-treatment data.
CONCLUSION. In individuals who are overweight or obese and have insulin resistance and prediabetes, activation of FXR by OCA results in enhanced insulin sensitivity. Patients who received OCA also lost weight.
CORRIGENDUM
A corrigendum on "A Rare Case of Co-occurrence of Multiple Endocrine Neoplasia Syndrome and Congenital Adrenal Hyperplasia" by Axenia S. Bondarenko, Elizaveta O. Mamedova, Zhanna E. Belaya, Galina A. Melnichenko (2024). Obesity and metabolism. 2024;21(1):79-84. DOI: 10.14341/omet13015.
On the page 82, the following text was added: "The presented case was first described in the dissertation of Kareva M.A. The author draws the readers' attention to the fact that the presence of CAH in the patient could lead to a delayed diagnosis of the second monogenic disease — MEN-1: episodes of indomitable vomiting in this case were considered as a manifestation of salt-wasting crises, but it cannot be excluded that they could be associated with the development of severe hypercalcaemia in the patient [30]".
A new source has been added in the reference list section under No. 30: «Kareva M.A. Vrozhdennaya disfunkciya kory nadpochechnikov u detej: epidemiologiya, geneticheskaya osnova, personalizirovannyj podhod k diagnostike i lecheniyu, monitoring somaticheskogo i reproduktivnogo zdorov’ya. [dissertation] Moscow; 2018. (In Russ)».
A corrigendum on "Androgen insensitivity syndrome: preventive gonadectomy, "pros" and "cons"" (Obesity and metabolism by Еvgenia A. Starostina, Nadezhda V. Frolkova, Seidbike M. Seidova, Elena G. Przhiyalkovskaya, Nadezhda M. Platonova (2024). Obesity and metabolism. 2024;21(1):85-91. doi: https://doi.org/10.14341/omet13024
On page 87 the sentence “In addition, testosterone preparations are used to treat infertility in patients with a mild form of STF [3]” was removed. Added paragraph “Birnbaum W et al. conducted a multicenter, double-blind, randomized, crossover study in three university medical centers and three specialized hospitals in Germany. In this study, patients aged 18-54 years with karyotype 46,XY, genetically confirmed CAIS, removed gonads, were treated with either estradiol drugs at a dose of 1.5 mg/day for 6 months, followed by a transition to testosterone 50 mg /day for 6 months (sequence A), or testosterone preparations 50 mg/day for 6 months, followed by a transition to estradiol 1.5 mg/day for 6 months (sequence B).
In the study, testosterone was well tolerated and as safe as estrogen. The authors suggested that testosterone may be an alternative replacement therapy for CAIS, particularly for patients with reduced sexual function."
A new source has been added in the reference list section under No. 30: “Birnbaum W, Marshall L, Werner R, et al. Oestrogen versus androgen in hormone-replacement therapy for complete androgen insensitivity syndrome: a multicentre, randomized, double-dummy, double-blind crossover trial. Lancet Diabetes Endocrinol. 2018;6(10):771-780. doi:10.1016/S2213-8587(18)30197-9.”
The authors regret the error. The original version of the article has been replaced.
REVIEWS
Rapid changes in the morphological characteristics of the population, which began in the middle of the last century, are due to changes in the habitat. The “obesogenic” environment that is formed in urbanized spaces contributes to physical inactivity and a hypercaloric diet, and the processes of globalization contribute to obesity in the population in all countries of the world. From the obesity epidemic declared by WHO in 1988, humanity has moved to an obesity pandemic. The presented review analyzes global and Russian trends in the development of obesity. Data on the prevalence of latent obesity and diagnostic criteria for this condition are presented. An analysis of data on the dynamics of BMI in the world and in the Russian Federation was carried out. Various options for the topography of fat deposition and their relationship with comorbid diseases are considered. The structure of the subcutaneous fat depot in the abdominal area and the influence of the outer (superficial subcutaneous abdominal adipose tissue, SSAT) and deep (deep subcutaneous abdominal adipose tissue, DSAT) layers of subcutaneous fatty tissue in the abdominal area on the risks of developing diseases are discussed. The results of assessing the diagnostic value of the T/A substitution in the FTO gene (rs9939609) for predicting the proportion of fat mass and abdominal fat deposition in adults are presented.
Hyperprolactinemia has multiple etiologies and is the most common endocrine manifestation of pathology of the hypothalamic-pituitary axis. Hyperprolactinemic hypogonadism is of great scientific interest due to the prevalence of endocrine pathology in the reproductive period and its effect on metabolic processes. Hyperprolactinemia is one of the serious obstacles to the implementation of reproductive function in both women and men. The article discusses current issues of diagnosis and management tactics for patients with hyperprolactinemia of various etiologies within the framework of preconception preparation.
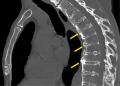
Acromegaly is a rare neuroendocrine disease caused by excessive production of growth hormone (GH), which acts as a trigger for cartilage tissue destruction leading to joint damage.
Patients with acromegaly, especially in the active stage, often complain of joint pain in various locations. Joint pain can be one of the first symptoms of the disease, the intensity of which worsens without proper treatment. Increased production of GH leads to configuration changes in the joints, which in turn trigger destructive processes typical of degenerative diseases such as osteoarthritis. Despite successful treatment of acromegaly, joint-related issues can persist and significantly worsen the quality of life for patients. In this regard, the search for potential markers of early joint involvement in acromegaly is relevant for use in predicting the severity of arthropathy progression and monitoring this cohort of patients.
This review provides a general overview of the effects of growth hormone on cartilage tissue, the characteristics of musculoskeletal pathology in patients with acromegaly and possible markers associated with early joint damage.
It has now been shown that overweight and obesity are associated with the development of at least 13 types of cancer, including cancer of the breast, colon and rectum, endometrium, esophagus (adenocarcinoma), gallbladder, stomach, kidney (renal cell), liver, ovaries, pancreas and thyroid glands, as well as multiple myeloma. Obesity-related cancers account for about 40% of all cancers. Thus, obesity is ahead of smoking as the most common modifiable risk factor for carcinogenesis. This review collects the latest data on the impact of obesity phenotypes on the risk of developing cancer, including a discussion of the contribution of the metabolically healthy obesity phenotype (MHO) to tumorigenesis. Possible mechanisms contributing to the emergence and progression of cancer are analyzed, for example: stimulation of cell proliferation, evasion of growth suppressors, inhibition of apoptosis and provision of replicative immortality, induction of angiogenesis, activation of invasion and metastasis, influence on genome instability, as well as chronic low-grade inflammation that contributes to the development of cancer. Understanding how obesity influences the above mechanisms may facilitate the development of new cancer prevention and treatment strategies for obese populations.
CLINICAL PRACTICE GUIDELINES
We recommend acromegaly to be ruled in all patients with characteristic changes in appearance (A3). In all patients without characteristic changes in appearance, we recommend to rule out acromegaly, if several clinical signs suspicious for acromegaly are present (B3). We recommend acromegaly to be ruled out in all patients with pituitary adenoma (B3). We recommend to rule out acromegaly in all patients with prolactin-secreting adenomas (C4). For laboratory confirmation of acromegaly, we recommend to measure serum insulin-like growth factor-1 (IGF-1, somatomedin C) level (A3). In patients without obvious clinical signs of acromegaly and/or with a moderate increase in IGF-1 levels (IGF-1 index less than 1.3), we recommend to assess the response of somatotropic hormone (GH) to hyperglycemia (GH during an oral glucose tolerance test) (B3). In all patients with biochemically confirmed acromegaly, magnetic resonance imaging of the pituitary gland with intravenous contrast is recommended to assess pituitary adenoma size, location and growth pattern (A3). We recommend to measure blood glucose and glycated hemoglobin in all patients with confirmed acromegaly (B3). We recommend to measure serum prolactin levels in all patients with acromegaly (B3).
In all patients with acromegaly and pituitary adenoma, transnasal transsphenoidal adenomectomy is recommended as first-line treatment if the patient’s consent is given and there are no contraindications (A1). For all patients with acromegaly for whom neurosurgical treatment is indicated, surgical intervention is recommended in medical centers, specializing in pituitary diseases, by neurosurgeons who perform at least 50 such operations per year (A3). We recommend that morphological and immunohistochemical examination of the removed pituitary adenoma is performed in all patients with acromegaly (A3). We do not recommend routine medical therapy for acromegaly before surgery as a mean to reduce tumor size (B2).
For patients with acromegaly in whom neurosurgical treatment is not indicated or ineffective or while patient awaiting for the effect of radiation therapy, we recommend medical therapy (A1). Long-acting first-generation somatostatin analogues are recommended as first-line drug therapy for acromegaly. In case of partial/complete resistance to or intolerance to somatostatin analogs, pegvisomant is recommended as a second-line medical therapy for acromegaly (A1). We recommend starting pegvisomant from a single dose of 40–80 mg per day subcutaneously, then continue injections at a starting dose of 10 or 15 mg per day with IGF-1 monitoring after 4–6 weeks and dose adjustment if necessary (B2). In patients with acromegaly and a moderate increase in IGF-1 levels, we recommend to initiate cabergoline as medical monotherapy or, if somatostatin analogs are ineffective, in combination with them (B2).
In patients with acromegaly, if the disease remains active after surgical treatment, if drug treatment is unavailable, intolerable or ineffective, and repeated neurosurgical intervention is inappropriate, it is we recommend radiation therapy (A1). A multidisciplinary approach is recommended in the management of acromegaly complications (C3).

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2306-5524 (Online)