NEWS
ORIGINAL STUDIES
BACKGROUND: Depending on the polymorphism of genes that that are involved in metabolism, the response of patients to different types of therapy may differ. Despite the potential effect of rs7903146 TCF7L2 and rs1042712 ADRB2 on changes in body composition in different types of therapy of early carbohydrate metabolism disorders, these associations haven’t been studied yet. AIM: To study the influence of rs7903146 TCF7L2, rs1042714 ADRB2 on changes in body fat composition in different types of therapy of early carbohydrate metabolism disorders.
MATERIALS AND METHODS: The study involved patients with overweight or obesity and risk factors for Type 2 Diabetes development. All patients underwent genotyping with the real-time polymerase chain reaction, oral glucose tolerance test and bioimpedancemetry. Further, the patients were divided into two groups. First group kept a diet with the exclusion of simple and limitation of complex carbohydrates and fats. Second group took metformin in addition to the diet. Three months after bioimpedancemetry was performed again.
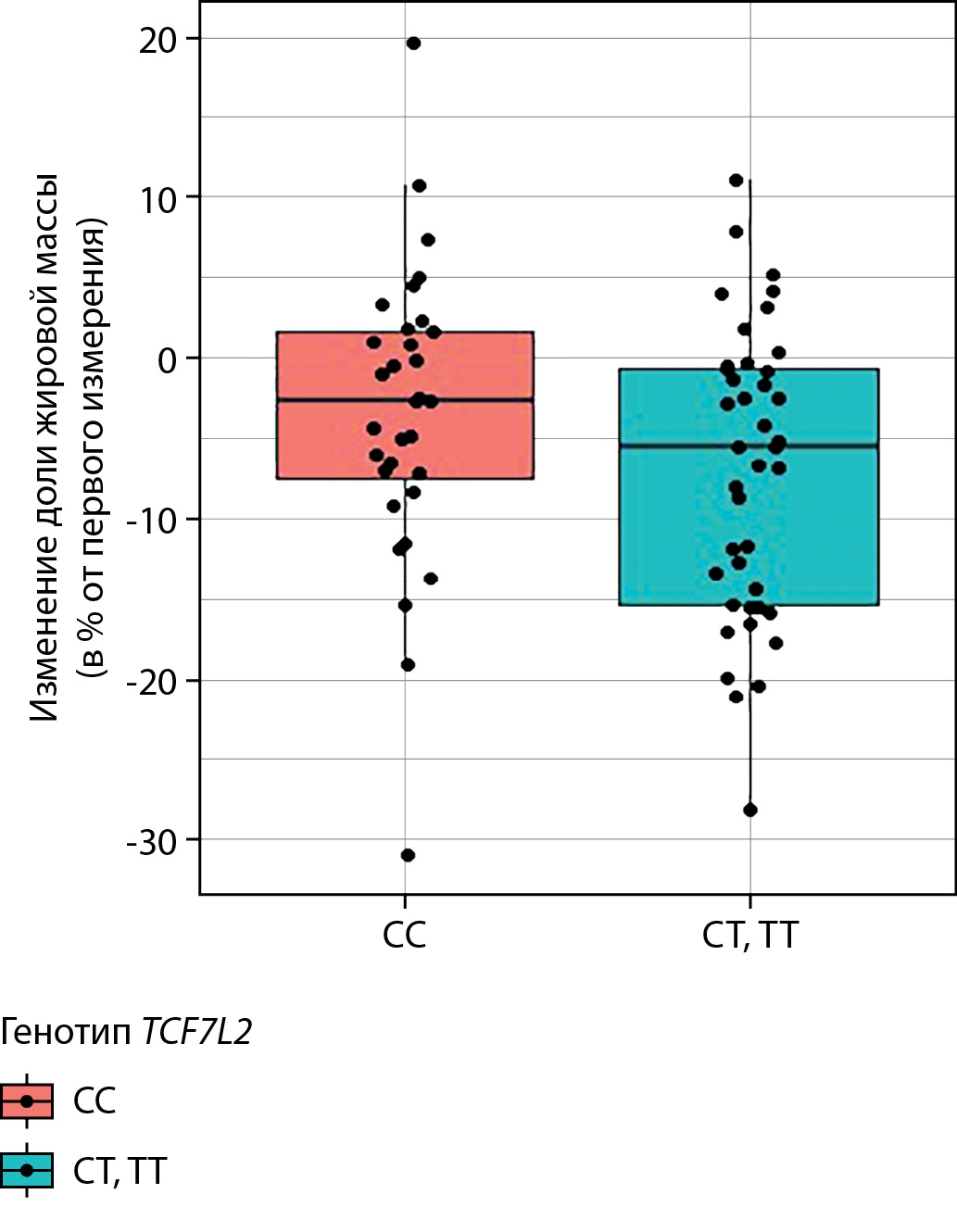
RESULTS: The research involved 73 patients (the mean age 48±12 y.o., the mean BMI 34,27±6,18 kg/m2 ). The diet therapy group consisted of 47 people. Other 26 patients took metformin in addition to the diet. In group of diet, T allele carriers of rs7903146 TCF7L2 were characterized with more decrease in fat mass compared with CC homozygotes (- 7.90 ± 9.46% vs. -1.54 ± 8.98%, p = 0.027). CC genotype carriers of rs7903146 TCF7L2 in group of metformin and the diet had a tendency for more decrease in hip circumference compared with T allele carriers (-4.95 ± 3.34% vs. — 2.5 ± 2.96%, p = 0.064). Carriers of C allele in homozygous state of rs1042714 ADRB2, who took metformin with the diet, demonstrated more decrease in hip circumference (- 5.81 ± 3.00% vs. -2.50 ± 2.7%, p = 0.009), the tendency for decrease in fat mass (-8.28 ± 8.86% vs. — 3.20 ± 5.09%, p = 0.068) and waist circumference (-5.91 ± 4.29% vs. -3.03 ± 4.01 %, p = 0.091) compared with G allele carriers. The association of rs7903146 TCF7L2 and rs1042714 ADRB2 with changes in total body weight was not observed (p> 0.05).
CONCLUSION: Single nucleotide polymorphisms rs7903146 TCF7L2 and rs1042714 ADRB2 influence on body fat composition in patients with early carbohydrate metabolism disorders in various types of treatment.
BACKGROUND: According to the involvement of oxidative stress in the pathogenesis of obesity, the plasma level of coenzyme q10 in the correlation relationship with lipid metabolism disorders and functional liver state is of interest to study.
AIM: Substantiation of approaches to the correction of lipid metabolism disorders and non-alcoholic fatty liver disease in children with exogenous obesity based on the content of coenzyme Q10 and its relationship with lipid profile and liver enzymes.
MATERIALS AND METHODS: The single-center cross-sectional study enlisted the control (n=32, -1.0≤BMI SD score ≤+2.0) and obese (n=40, BMI SD score>+2.0) groups of children with the mean age of 12 yr. In all children BMI, lipidogram, liver enzymes (ALT and AST), plasma coenzyme Q10 and liver ultrasound examination were assessed.
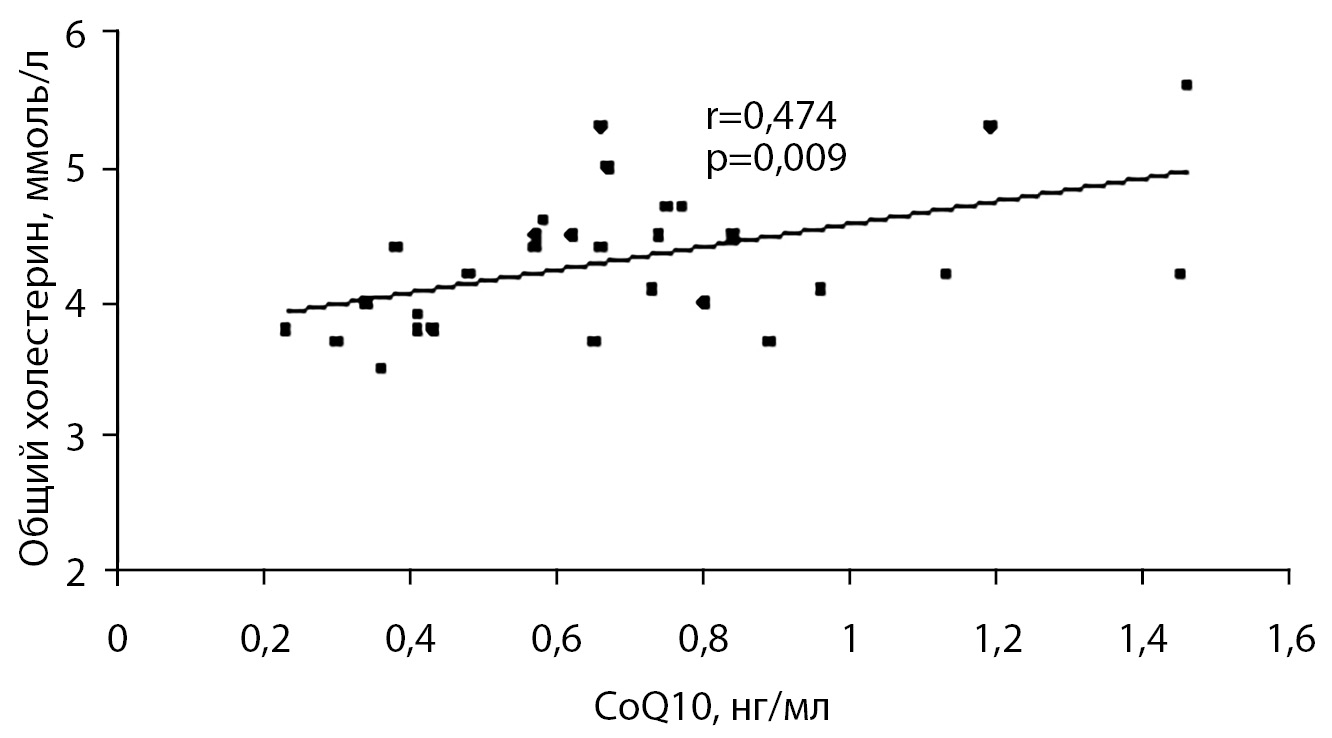
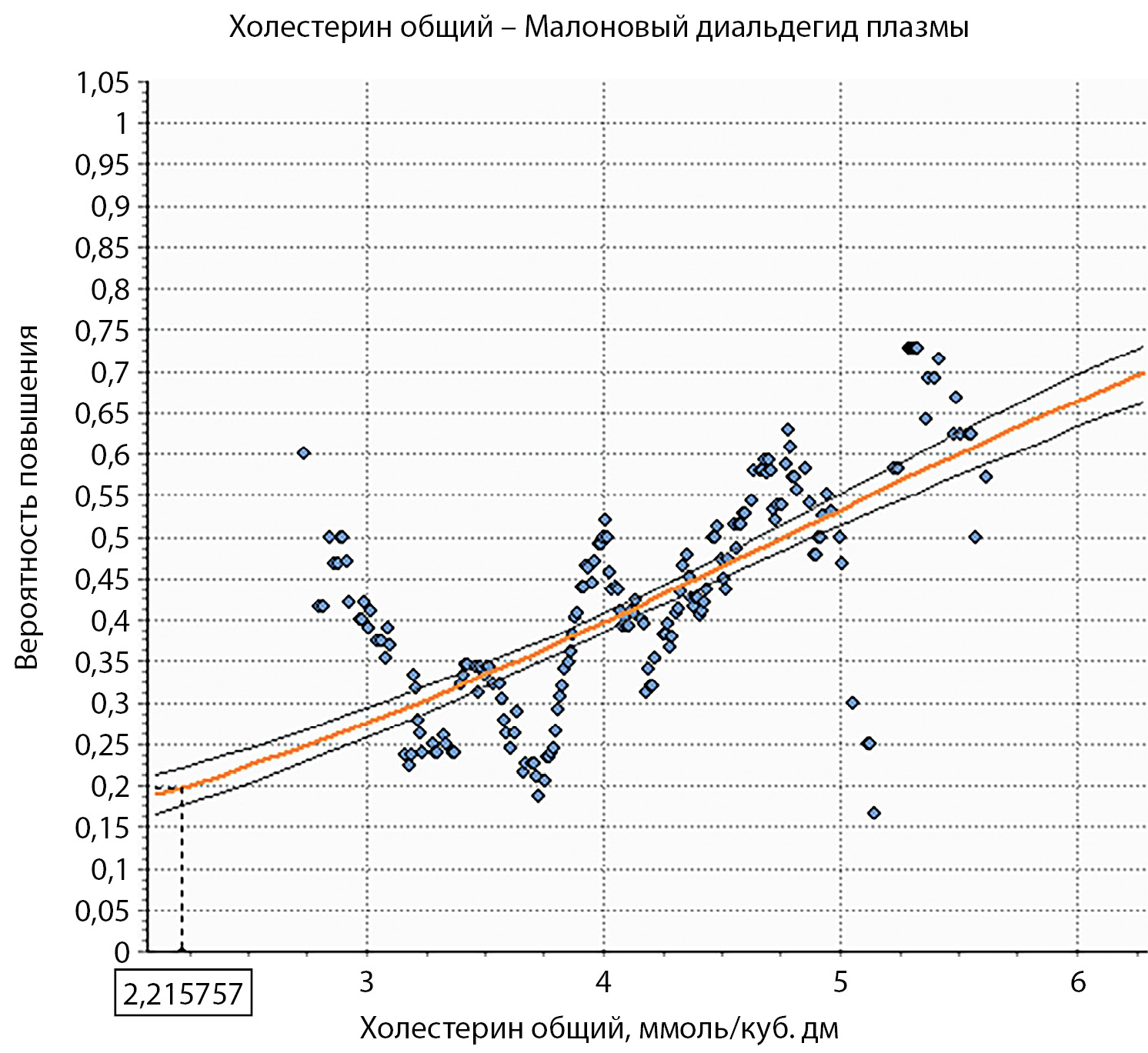
RESULTS: Patients of both groups were comparable (p> 0.05) in age and gender. The level of coenzyme Q10 in the compared groups was comparable (p> 0.05) and did not differ in patients with different degrees of obesity. According to the results of the study of the lipid profile in the obese children, the level of HDL was lower, and the level of LDL was higher than that in control group. The highest value of HDL was obtained in the patients with the 1st degree of obesity and the highest level of triglycerides — in the patients with the 4th degree of obesity. The control group demonstrated moderate correlations between endogenous coenzyme Q10 and total cholesterol (r=0.474, p=0.009) which persists in patients with the first degree of obesity (r = 0.548, p = 0.035). There was no difference in AST in the study groups, however, the main group demonstrated elevated ALT and ALT/AST ratio (p <0.001). The highest ALT and ALT / AST ratio were observed in patients with greatest degree of obesity. Eighteen obese children (45%) had ALT / AST ratio ≥1 (in the control group –one patient (3%) (p <0.001), while fourteen patients showed liver enlargement and structure change according to ultrasound (80%). The control group demonstrated moderate correlations between endogenous coenzyme Q10 and total cholesterol (r=0.474, p=0.009) and between coenzyme Q10 and ALT / AST ratio (r=0.412, p=0.023) . In the obese group there was correlation between AI and ALT / AST (r = 0.436, p = 0.006) and in patients with the 1st degree of obesity — between also coenzyme Q10 and ALT (r = 0.875, p <0.001).
CONCLUSION: The disturbances in adequate control of cholesterol by coenzyme Q10 in obese children possibly confirming the involvement of oxidative stress in the pathogenesis of dyslipidemia and non-alcoholic fatty liver disease can serve as indication to use coenzyme Q10 in order to correct these complications.
BACKGROUND: Essential arterial hypertension (AH) develops more often in children with accompanying risk factors — obesity, overweight, positive heredity and genetic predisposition.
AIM: Study of peculiarities of arterial hypertension clinical course in adolescents with normal body weight, overweight and obesity.
MATERIALS AND METHODS: The study was conducted on children with arterial hypertension who received treatment in two hospitals in Voronezh in 2016–2020. A retrospective analysis of the children’s case histories was carried out taking into account the anamnesis, clinical laboratory and instrumental examination data and the pharmacotherapy. Some children underwent polymerase chain reaction genetic testing to determine pathological alleles of genes regulating blood pressure (BP).
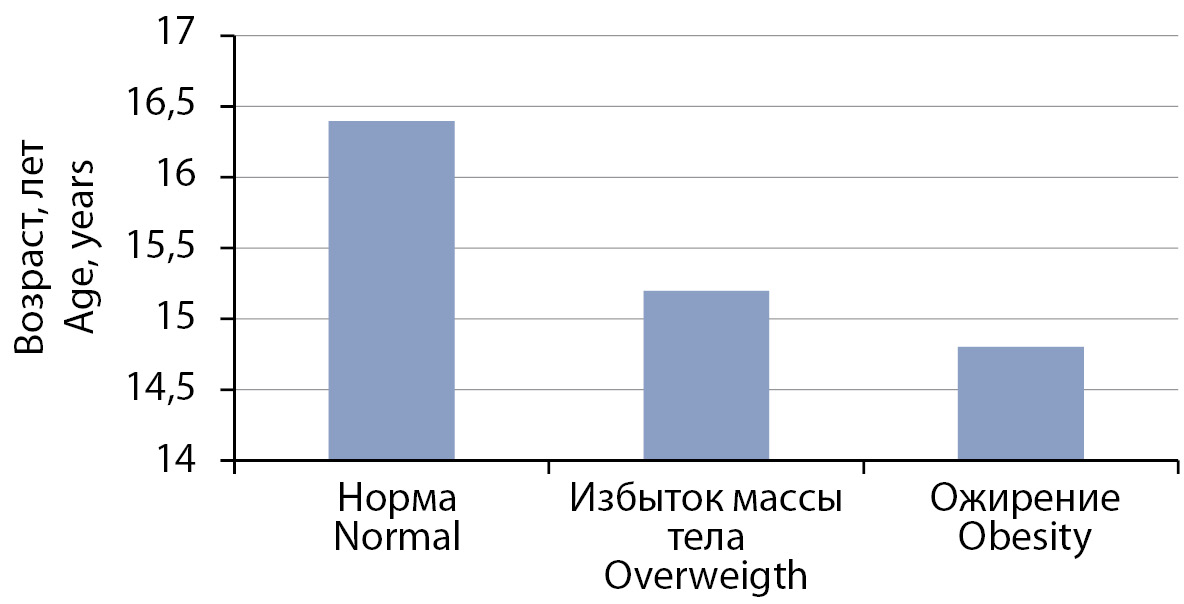
RESULTS: 96 patients aged 9 to 17 took part in the study. The group with normal body weight included 38 children (39.6%), median age 16.4 (aged 10.7; 17.9), with overweight — 33 people (34.4%), median age 15.2 (aged 12.0; 17.9), with obesity — 25 children (26.0%), median age 14.5 (aged 9.2; 17.9). Obese children developed arterial hypertension at earlier age (p = 0.023). According to blood pressure daily monitoring (BPDM), pathological values of systolic blood pressure (SBP) during the day (above the 95th percentile) among children with normal body weight were observed in 17 patients (44.7%), with excess body weight — in 14 people (42.4%), with obesity — in 16 people (64%), p = 0.031. Accurate difference values between the groups were obtained in terms of time index (TI) of SBP at night (p = 0.006). Time index of diastolic BP during the day > 50% was observed only in the obese children group — 4 people (16%) (p = 0.042). Pathological alleles of the angiotensinogen gene (AGT: 704 T>C), aldosterone synthase gene (CYP11B2: -344 C>T) and endothelial nitrogen synthase type 3 (NOS3: -786 T> C) were identified most frequently during genetic testing in some patients.
CONCLUSION: Children with obesity developed earlier arterial hypertension compared to the same-age children with normal body weight and more often had unfavorable type of arterial hypertension according to BPDM. These results can be used to choose individual therapy and to develop special attention as regards certain target organs damage.
BACKGROUND: An increase with age in the blood glucose level of permanent residents of the Arctic region is a risk factor for metabolic changes, including diabetes mellitus (DM), the frequency and prevalence of which is often accompanied by an increase in body weight and obesity. However, at the moment, there is no clear idea of the age range in the structure of metabolic changes in northerners, and the influence of gender on the content of glucose, its metabolites, pancreatic hormones and the nature of the relationship between them in adults requires clarification.
AIMS: To assess the values of the parameters of carbohydrate metabolism, pancreatic hormones, body mass index and the nature of the relationships between them in residents of the Arctic region who were born and permanently residing in the Nenets (NAO), Yamalo-Nenets Autonomous Okrug (Yamalo-Nenets Autonomous Okrug (Yamalo-Nenets Autonomous Okrug) and Mezen District of the Arkhangelsk Region, taking into account gender and age.
MATERIALS AND METHODS: In the blood serum healthy residents of the NAO, YaNAO and the Mezensky district of the Arkhangelsk region of mature age, born and permanently residing in the Arctic region, randomly selected after a medical examination and questioning, which depending on gender and age were divided into groups: women 21–35, 36–45, 46–55 years old and men 22–35, 36–45, 46–60 years old. The blood serum was determined by the content of glucose, lactate, pyruvate, insulin, proinsulin, C-peptide was determined, measured height and weight.
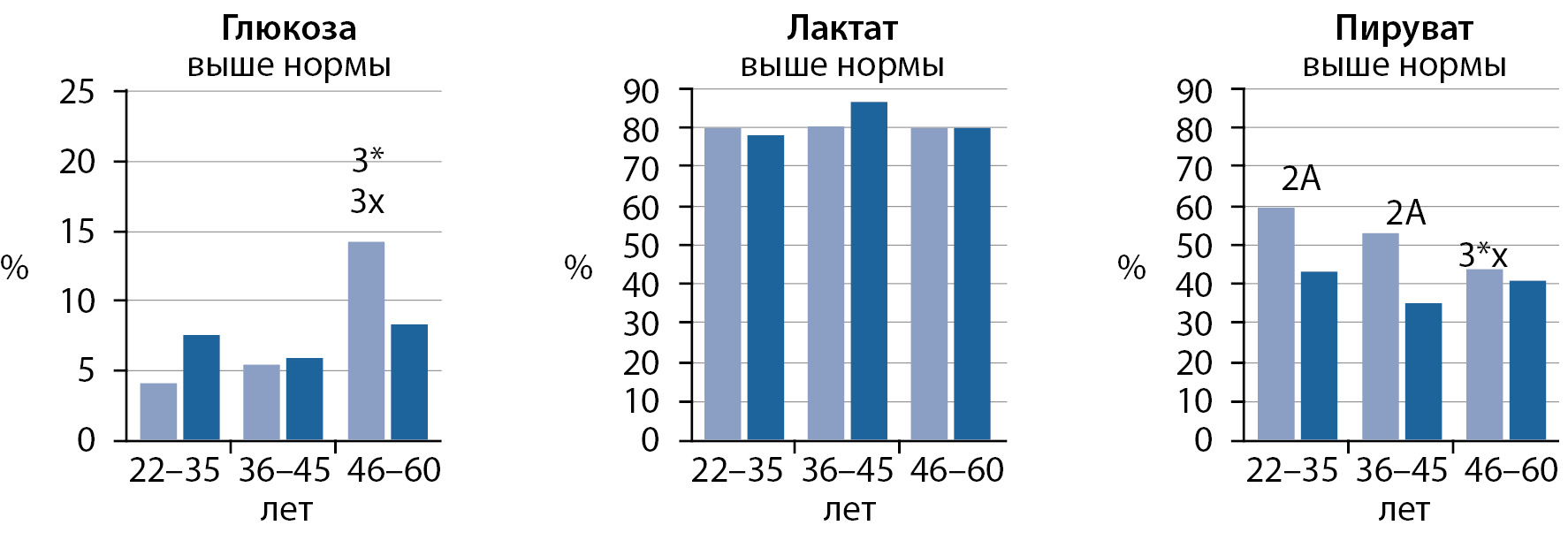
RESULTS: The study involved 1146 people of mature age (women 21–35 (221), 36–45 (222) and 46–55 (371), men 22–35 (105), 36–45 (84), 46–60 (143) years). Regardless of gender, the content of glucose (Glu) significantly increases with age, the peak of which occurs in women aged 46–55 years and in men aged 46–60 years. Age-related changes in the content of lactate (Lac) and pyruvate (Pir) were not found, but in men aged 36–45 years, the level of Lac was higher than in women, and the content of Pir, on the contrary, in all age groups, regardless of gender, was shifted to the lower limit of normal and below it. Against the background of an increase in Glu in women aged 46–55 years the level of insulin was significantly increased, and in men aged 46–60 years, the level of proinsulin was significantly increased. The value of the HOMA index, regardless of gender, exceeded the norm, and the value of the Caro index was below the critical level, which indicates hidden disorders of carbohydrate metabolism.
CONCLUSIONS: In permanent residents of the Arctic region (NAO, YaNAO, Mezensk district of the Arkhangelsk region) of mature age, sex differences were established in the content of glucose, lactate, pyruvate and in the regulation of insulin-stimulated glycolysis by pancreatic hormones, as well as an excess of the BMI norm in 50,9, 67,0, 75,0% of women and 52,1, 66,6, 63,7% males.
BACKGROUND: Recently, there has been an increase in the number of cardiovascular diseases and mortality rates among the population. This may be due to a violation of metabolic processes in the body, in particular lipid and carbohydrate metabolism, caused by an unbalanced high-calorie diet.
PURPOSE: To study and compare the main indicators of carbohydrate and lipid metabolism in a fructose-fortified diet and a diet with a high fat content under experimental conditions.
MATERIALS AND METHODS: The study was carried out on outbred white rats, males, which were divided into 3 groups — a control group and two experimental ones, 15 individuals in each. The rats of the first experimental group were kept on a high-fat diet, the second experimental group was assigned a fructose-enriched diet for 35 days. The control group was on a balanced diet. We studied the changes in the parameters of carbohydrate (glucose, insulin, insulin resistance indices) and lipid (cholesterol-, high- and low-density lipoproteins, triglycerides) metabolism on the 21st, 35th and 60th days of the experiment. The results were statistically processed using the Mann-Whitney test. The study design is retrospective.
RESULTS: During the experiment, an increase in the content of glucose, insulin, and lipid metabolism parameters was observed in the experimental groups. Moreover, the content of glucose and insulin in a fructose-fortified diet increased by 18.7% (p = 0,009), 22.2% (p = 0,076), 21.5% (p = 0,009) and 50% (p = 0,009), 62.5% (p = 0,009), 106.3% (p = 0,009) over the days of the experiment, respectively. The increase in lipid metabolism was more pronounced in the experimental group, which had an increased fat content in the diet, already in the first time period of the experiment: cholesterol — by 80,8% (p = 0,009), low-density lipoproteins — by 100% (p = 0,009), triglycerides — by 120% (p = 0,009), high-density lipoproteins — by 60.9% (p = 0,009).
CONCLUSION: The experimental data obtained show changes in lipid and carbohydrate metabolism due to increased consumption of fats and fructose.
BACKGROUND: There are a lot of works devoted to the study of the main regularities of the heart rate (HR) control in individuals depending on the body weight. Still, there are some uncleared and even controversial issues that significantly influence the notion of this process itself. Particularly, impaired HR variability in patients with the cardiometabolic syndrome is characterized by the weakening of the impact of both parasympathetic and sympathetic branches of the autonomic nervous system. The works devoted to the heart rate variability features in young people associated with the body weight are scarce.
AIM: To study the peculiarities of the heart rate variability in boys and girls with different body composition, motor and eating behavior.
MATERIALS AND METHODS: A cross-sectional, open, single-arm, non-randomized study of the HR variability in adolescents with different body fat mass (BFM) was carried out on the basis of the Center for Healthy Nutrition of Altai State University. The HR variability, nutritional status and physical activity index (PHAI) were studied in the groups of individuals with different body fat mass.
RESULTS: We examined 168 people (85 boys and 83 girls). The surveyed belonged to the adolescent age period (boys from 17 to 21 years old, girls from 16 to 20 years old). The boys and girls examined by us had a different amount of BFM %. The HR variability, nutritional status and physical activity index were studied in 44 people with the low BFM, 71 people with the average BFM, 53 people with the increased BFM. In both sexes, the group with the increased BFM features an increase in the absolute (HF, ms2 ) and relative (HF%) oscillation power of the heart rate high-frequency component. The average value of the physical activity index in the group with the reduced BFM equals 1.52 ± 0.037 in boys, and 1.44 ± 0.099 in girls. The average value of the physical activity index in the group with the average BFM is 1.44 ± 0.029 and 1.42 ± 0.095 in boys and in girls respectively. The average value of the physical activity index in the group with the increased BFM is 1.23 (Q25–75 1.20–1.70) in boys, and 1.26 ± 0.33 in girls. The representatives of the group with the increased BFM have a higher caloric value (CV) of the daily intake. In young men, a higher CV was achieved due to increased consumption of fats and carbohydrates. In the girls of the third group, a higher CV of the daily intake was gained due to proteins, fats, carbohydrates.
CONCLUSION: The results of the HR variability showed that the motor and eating behavior affect the state of the cardiac function in both boys and girls. An increase in the body fat mass in the individuals with a maximum CV of the daily intake and a minimum level of motor activity is associated with the prevalence of the parasympathetic branch of the autonomic nervous system in the heart rate control.
BACKGROUND: In the Russian Federation, the incidence of obesity continues to grow among the child population. Vegetative imbalance and chronic stress play an important role in the pathogenesis of obesity and related health disorders. Timely identification of disorders of psycho-vegetative disorders and their correction in overweight children require an integrated approach of medical and pedagogical workers.
AIM: To reveal the features of the vegetative status, the level of school anxiety in students with an increased body mass index.
MATERIALS AND METHODS: Children with different body mass index (BMI) underwent a comparative analysis of the mean values and structure of revealed violations of cardiointervalography (heart rate variability, HRV) parameters, laboratory test parameters (plasma antioxidant activity, plasma malondialdehyde, triglycerides, total cholesterol, cortisol, magnesium and serotonin) and test parameters School Anxiety Scale of Phillips.
RESULTS: The prevalence of overweight was 23.1%. The observation group consisted of 47 schoolchildren with a body mass index (BMI) +1–2 SD the comparison group consisted of 156 children with a normal BMI at the age of 10–15 years. The groups were comparable in terms of sex and age (p=0.629–0.771). Analysis of background HVR indices revealed a decrease in the values of parameters characterizing the activity of the parasympathetic division of the autonomic nervous system (ANS), with a simultaneous increase in the indicators of the sympathetic division of the ANS in the observation group relative to the comparison group (p=0.001–0.023); similar results were obtained during the orthostatic test. The cumulative assessment of CIG indicates a lower activity of the parasympathetic division in the regulation of the state of rest and a greater activity of the sympathetic division of the ANS in response to a stress factor in children with an increased BMI value. The children of the observation group showed higher levels of malondialdehyde (p = 0.041), triglycerides (p<0.001) and cortisol (p=0.093) with lower values of magnesium and serotonin (p=0.074–0.076). The analysis of the level of school anxiety showed that in children of the observation group the average level and frequency of the prevalence of high values of the indicator of general anxiety are higher in 1.3 and 2.5 (p=0.005), fear of self-expression — in 1.3 and 1.8 (p=0.080–0.086), fear of the situation of knowledge testing — by 1.5 (р=0.002) and 2.1 (p<0.001), the level of general anxiety — by 1.2 (р=0.090) and 2.3 times (p=0.036) relative to the comparison group. In the course of the mathematical analysis, the results were obtained indicating the relationship between the parameters of the vegetative and psychological status.
CONCLUSION: The problem of excess nutrition remains an urgent issue of modern health care. Excess body weight is accompanied by the activation of the sympathoadrenal system with an increase in the level of school anxiety and all together forms a vicious circle. Excessive nutrition in school-age children requires an integrated approach of specialists in the medical and psychological-pedagogical sphere.
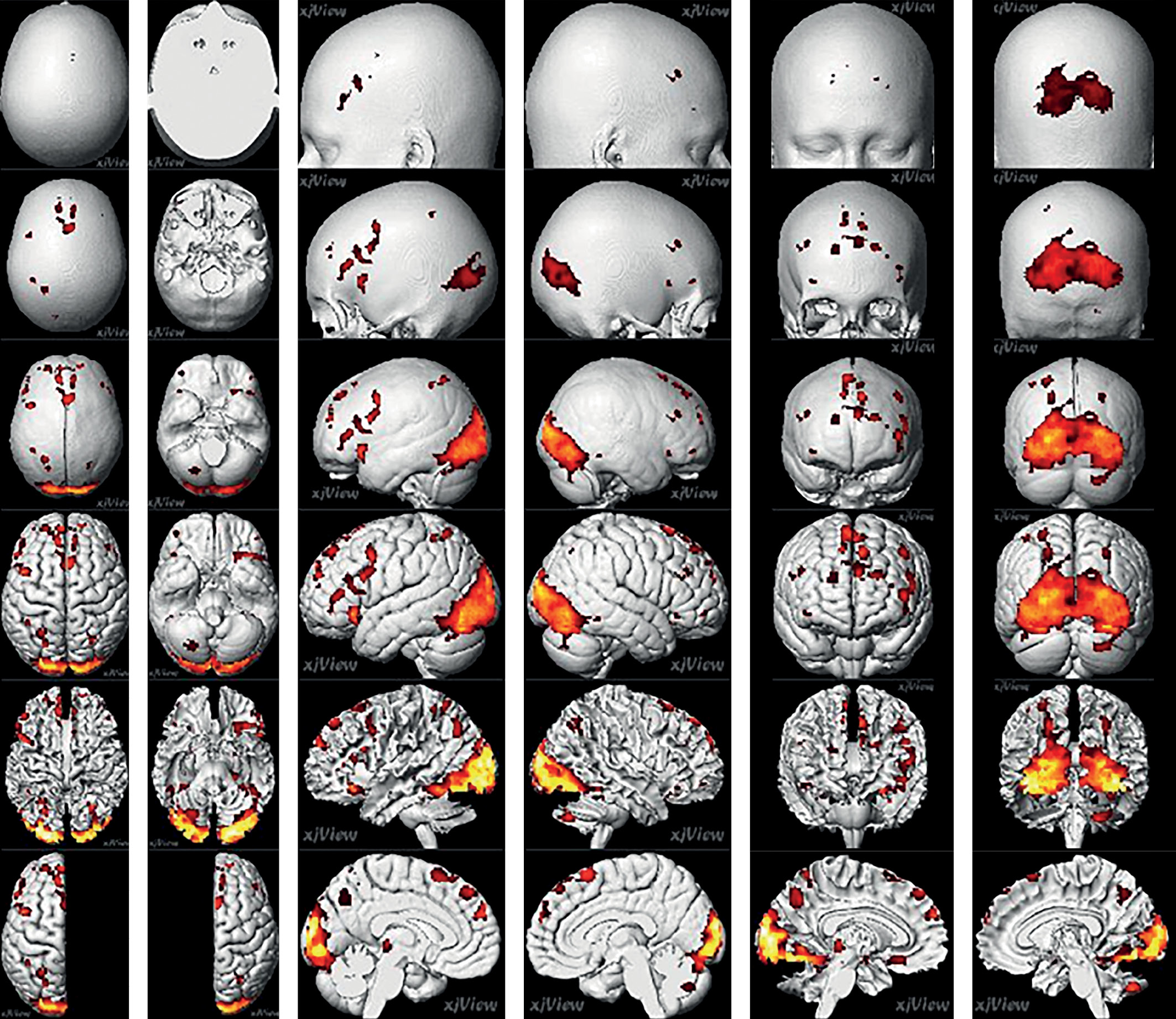
AIMS. Study of the dynamics of brain activity using functional MRI (fMRI) in obese patients treated with sibutramine (Reduxine®).
MATERIALS AND METHODS. The study enrolled patients with a body mass index (BMI) ≥30 kg/m2 . All participants underwent initial brain fMRI mapping. The obesity cohort was treated with sibutramine at a dose of 10 or 15 mg per day for 3 months. After treatment patients with obesity underwent a second fMRI mapping to assess changes against the initial mapping.
RESULTS. The study included: 30 patients (86,7% women) with mean age of 31 [27.25; 36] years, mean body weight (BW) - 106 [95.75; 121.75] kg, mean BMI 37.4 [33.55; 41.9] kg/m2 , mean waist circumference (WC) - 109 [100; 114.75] cm. The most marked activation volume (via fMRI) was observed in patients with obesity (before treatment) in the visual cortex (occipital lobes). After 3 months of treatment with sibutramine, 80% of patients lose ≥5% of BW. Mean BW decrease was -7.2 [-13.46; -5.37] kg, BMI decrease — -7.2 [-13.49; -5.34] кг/м2 , WC decrease — -6.9 [-11.88; -4.03] см, p <0,05. According to fMRI data, a decrease in brain activation in the projection of the occipital lobes (35%), left insula (44%), and increase inactivation by 70% in the area of the left DMPF.
CONCLUSION. A dynamic study of brain activity using fMRI in obese patients showed that during treatment with sibutramine, a decrease in body weight is accompanied by a decrease in activation in the projection of the occipital lobes and the left insular lobe of the brain, and an increase in activation in the area of the left DMPFC. These data may indicate a decrease in the emotional perception of high-calorie food, a decrease in motivation to eat it, and an increase in cognitive control. In general, the noted dynamics of the functional activity of the brain in obese patients against the background of obesity therapy can be regarded as a change in previously formed patterns of eating behavior.
BACKGROUND: With the development of visceral obesity, against the background of insulin resistance (IR), lipo- and glucose toxicity in tissues progresses, which disrupts the metabolic balance of the body, and is the main factor in the development of type 2 diabetes mellitus (DM2). To date, a growing number of publications highlighting the role of circadian rhythms in the control of gluconeogenesis and lipogenesis. In the context of the development of DM2, the process of rhythm mismatch (desynchronosis) is increasingly mentioned, for the diagnosis of which the calculation of amplitude-phase parameters is used. Thus, the study of circadian rhythm disturbances using amplitude-phase parameters and factors influencing them is of particular interest in individuals with visceral obesity and prediabetes, since the data obtained can be used as markers for preclinical diagnosis of DM2.
AIM: To identify significant differences in the parameters (amplitude, acrophase) of circadian rhythms (fasting glycemia, basal body temperature, heart rate) as markers of desynchronosis in groups without carbohydrate metabolism disorders, but with the presence of visceral obesity, prediabetes (impaired fasting glycemia, impaired glucose tolerance test) and DM2 and obesity.
MATERIALS AND METHODS: The study was conducted in individuals with visceral obesity, as well as the presence of prediabetes or DM2, with a disease experience of not more than 5 years.In accordance with the study design, every 3 hours during the day, the participants made self-measurements of blood glucose at home (using individual glucometers), basal body temperature (BTT) in the armpit (using a mercury thermometer) and heart rate (HR) ( with the help of an electronic tonometer), with the fixation of the results in self-control diaries. To assess the reliability of the circadian rhythms of the studied indicators, the interpretation of chronobiological parameters (MESORa-Midline Estimating Statistic of Rhytm; amplitude; acrophase) was carried out using a single сosinor analysis.
RESULTS: Of the 120 study participants, 73% were women and 27% were men. Mean age of participants was 58.6[52.2;56.7] years, BMI 31.3[29.7;33.9] and presence of visceral obesity WC 100 [93.8;104.7]. When conducting cosinor analysis, the daily rhythms of physiological indicators of fasting glycemia, BTT and heart rate differ from normal already in the group with visceral obesity without carbohydrate metabolism disorders and prediabetes, in the form of a decrease in the amplitude of daily rhythms (p<0.001), with a shift in their acrophases (p <0.001), no dynamics of night BBT decrease (р<0.001).
CONCLUSION: Integral amplitude-phase parameters of circadian rhythms of physiological parameters (fasting glycemia, basal body temperature, heart rate), as markers of desynchronosis, can be used in the presence of visceral obesity for preclinical diagnosis of prediabetes and DM2, which will have a preventive focus. This method of chronodiagnostics can be useful in health and prevention centers for people at risk of developing DM2.
CASE REPORT
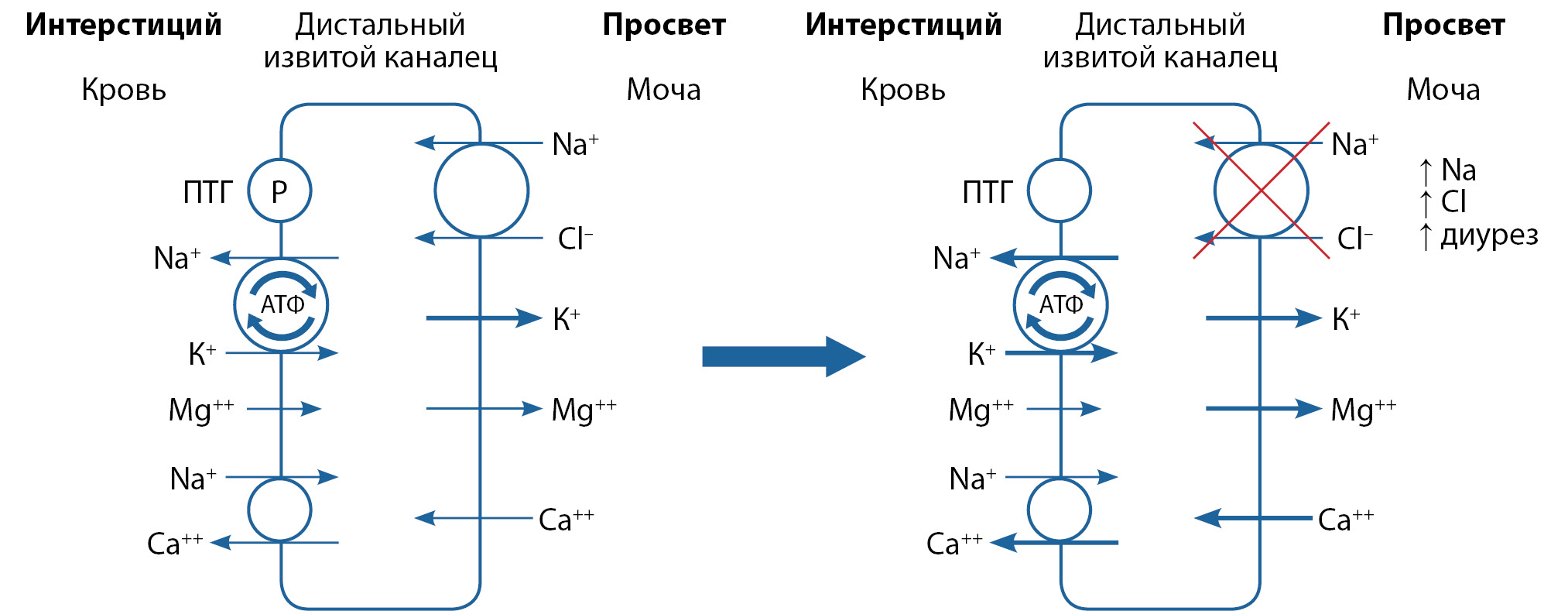
Hypercalciuria is a pathological condition characterized by an excess of daily calcium excretion. A high concentration of urine calcium can initiate stone formation. There are several types of hypercalciuria, each requires an individual approach. In the absence of known causes of development, idiopathic hypercalciuria is a frequent dysmetabolic disorder defined as an excess urine calcium excretion with normocalcemia. Resorptive hypercalciuria most often develops due to primary hyperparathyroidism and is caused by elevated PTH and excess release of calcium from bone stores. A thiazide test can be used for differential diagnosis between these conditions. We present a series of clinical cases covered the thiazide test in outpatient practice. The definitive diagnosis is extremely important because it determines the optimal treatment strategy. Secondary hyperparathyroidism (an increase in parathyroid hormone as a result of vitamin D deficiency, chronic renal failure or other conditions) requires medical therapy, while the primary hyperparathyroidism is radically cured only after surgical intervention.Taking into account the prevalence of idiopathic hypercalciuria and primary hyperparathyroidism, it is actual to use the thiazide test more widely in clinical practice.
REVIEWS
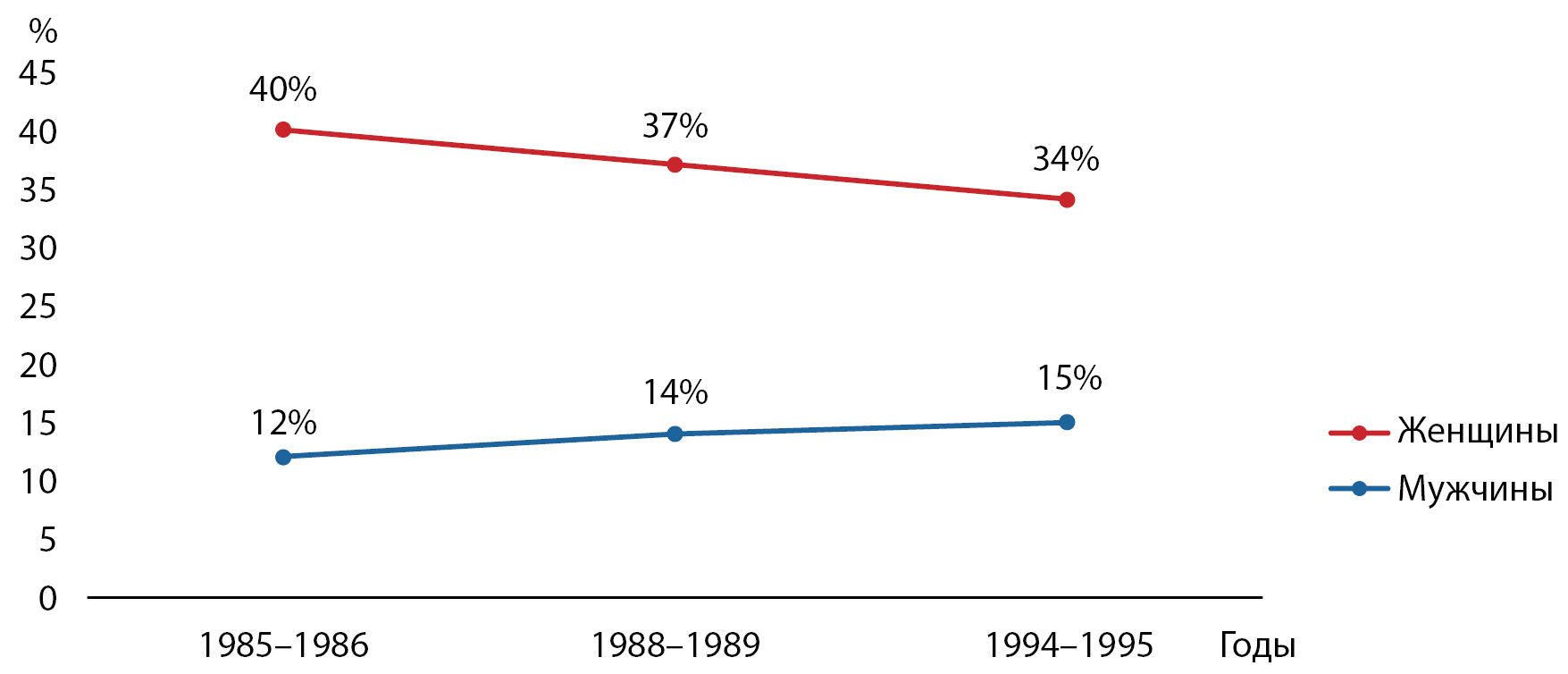
This review analyzes the prevalence of obesity among the adult population in the Russian Federation. The data of various studies, including large international projects (WHO MONICA 1985–1995, HAPIEE 2003–2005), all-Russian screenings (RLMS - HSE 1993, Federal monitoring of arterial hypertension 2003, ESSE-RF 2013 — present.), as well as selected regional studies. In some regions, the long-term dynamics of obesity has been studied. The history of studying the epidemiology of obesity in Russia has more than thirty years. According to the data obtained, the prevalence of obesity throughout the country remains high and continues to increase. Thus, among men, the prevalence increased from 10.8% in 1993 to 27.9% in 2017, among women — from 26.4% to 31.8%, respectively. In all regions where it was possible to assess long-term trends, the prevalence of obesity among adults increased (maximum — 48.5% in the Belgorod region). In the adult population, obesity is more common in women (maximum — 47.0% in the Novosibirsk region) than in men (maximum — 30.0% in Ivanovo and Voronezh regions). It is necessary to expand the number of regions in Russia in which studies of the prevalence of obesity are carried out, as well as to strengthen measures to combat overweight and obesity in all age groups throughout the country.
In the modern world, fast food is becoming part of the food culture; herewith, children and teenagers are no exception. A fairly busy lifestyle and lack of time contribute to an increasingly frequent appeal to fast food outlets. Given the national health policies of many countries, including those aimed at keeping up and supporting healthy lifestyles among children and adolescents, the researchers are increasingly focusing on the dependence of obesity on the younger generation’s fascination with fast food. In the proposed review, the authors have analyzed the published data represented in the studies at various levels and regarding a few problems. They are: the establishment of the relationship between a systematic intake of fast food and obesity among children and adolescents; the influence of the distance of fast food outlets from educational institutions on the occurrence and development of metabolic pathologies. Taking into consideration the relationship between fast food consumption by children and adolescents, parents and schools should strictly control their intake of unhealthy foods that leads to the weight gain and obesity-related diseases. Stopping marketing of junk food targeted at kids with eye-catching advertising personalities and gifts, could be one of the ways of childhood’s nutrition revitalizing.
The main goal of bariatric surgery is weight loss due to fundamental differential changes in the anatomical and physiological characteristics of the gastrointestinal tract. At the same time, one of the most frequent complications of obesity surgery, especially operations associated with malabsorption, is vitamin D deficiency. Patients with obesity initially have a wide range of predisposing factors for metabolic diseases of the skeleton due to lifestyle problems. Nutrient deficiencies with high-calorie diets and a sedentary lifestyle with a tendency to wear clothing that covers most of the skin — reduces serum 25 (OH) D levels. In addition, the situation is aggravated by a decrease in the bioavailability of 25 (OH) D due to its sequestration in adipose tissue and its complete inaccessibility to the central blood flow. The consequences of bariatric surgery — a decrease in the amount of skin and malabsorption can aggravate the existing deficiency. As a result of a decrease in the level of 25 (OH) D and subsequent hypocalcemia and secondary hyperparathyroidism, negatively affect the state of bone health. The presented literature review is devoted to the problems of obesity surgery and vitamin D deficiency. The main focus is on bone metabolism associated with bariatric surgery, the causes of pre and postoperative vitamin D deficiency are discussed, and recommendations for its treatment after obesity surgery are given.
Over the past decades, we have witnessed many remarkable advances in understanding the impact of vitamin D on human health. There is an exponential growth of new data covering both the fundamental biology of vitamin D and the clinical implications of deficiency and the effects of vitamin D supplementation. This literature review has been prepared to combine and interpret the current scientific evidence on the mechanisms of vitamin D absorption, with a focus on vitamin D absorption through the apical membrane of enterocytes in various pathologies of the gastrointestinal tract. Reviewed studies have identified some distinctive aspects of vitamin D bioavailability that should be considered in the treatment or prevention of vitamin D deficiency in patients with malabsorption syndromes, especially in the active phase of the disease. Moreover, recent in vivo experiments and in vitro studies have demonstrated that vitamin D absorption is not a simple diffusion process as previously thought, but rather a mechanism that also involves multiple membrane transporters. Maintaining or improving vitamin D intake through diet or increased sun exposure is problematic, so oral supplementation may be an effective and safe approach to improving vitamin D status. Vitamin D3 is the recommended form for both prevention and treatment of vitamin D deficiency, which is associated with more stable pharmacokinetics. Vitamin D absorption is improved when vitamin D is taken with a small amount of fat-containing food and medium chain triglycerides. In malabsorption syndromes, it is optimal to increase the general population doses of vitamin D by 2–3 times both for prevention and for the treatment of deficiency and insufficiency. While vitamin D deficiency is more common among people with gastrointestinal disease, data have not been able to establish whether the relationship is causal or the result of intestinal inflammation and malabsorption syndrome. However, owing to the understanding of the mechanisms of action of vitamin D, there is evidence that its deficiency can be directly related to the severity of the disease, and partly to the etiology or pathogenesis of the disease itself.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2306-5524 (Online)