NEWS
ORIGINAL STUDIES
AIM: assessment of the diagnostic accuracy of a 3% hypertonic saline infusion test in relation to a set of clinical and laboratory data (including a water deprivation test and MRI data) for differential diagnoses of diabetes insipidus (DI) and primary polydipsia (PP).
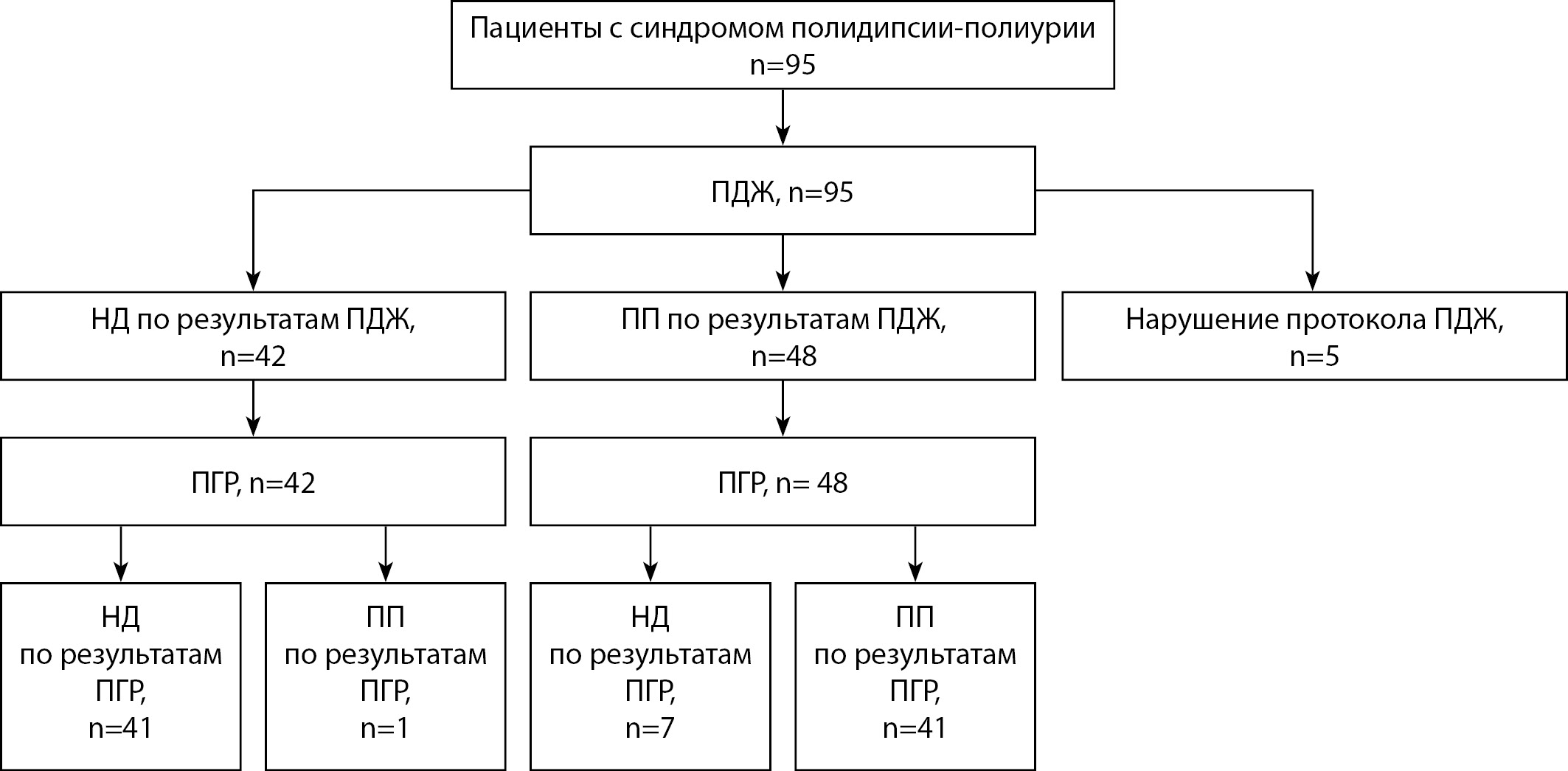
METHODS: An interventional cross-sectional study was carried out at Endocrinology Research Centre From September 2021 to September 2023 ninety patients with polyuria-polydipsia syndrome were included. In order to assess the diagnostic characteristics, all the subjects underwent two tests with osmotic stimulation: a 3% hypertonic saline infusion test and a water deprivation test. Adverse events were assessed.
RESULTS: Based on the results of clinical, anamnestic, laboratory and instrumental data, and the results of a water deprivation test, a final diagnosis of DI was made in 48 (53%) patients and PP in 42 (47%) patients. The agreement between the two samples is significant — Kappa = 0.823, 95% CI (0.707, 0.939). The operational parameters of the 3% hypertonic saline infusion test are: sensitivity 98% (95% CI: 89%; 100%); specificity 98% (95% CI: 87%; 100%), positive and negative predictive values 98% (95% CI: 89%–100%) and 98% (95% CI: 87%–100%). Respectively. Chills occurred significantly more often (31% vs. 12%), and dizziness and headache were more pronounced during the 3% hypertonic saline infusion test. The median duration of the water deprivation test in patients was 11 hours, and median duration of 3% hypertonic saline infusion test was 1.5 hour (P<0.001).
CONCLUSION: The 3% hypertonic saline infusion test has a high overall diagnostic accuracy 98%; 95% CI 92% to 100%)) in relation to the classical set of clinical, laboratory and instrumental data of patients (including a water deprivation test), However, it is important the advantage of the latter is its short duration and, as a consequence, better tolerability and probably better compliance, while no significant differences in adverse events frequencies during the tests were identified.
BACKGROUND: Diabetes mellitus and obesity are two closely related diseases that are a global public health problem. Obesity is characterized by an increase in the volume of adipose tissue and a change in the production and function of adipocytokines, which leads to a violation of the regulation of insulin sensitivity and glucose metabolism, contributing to the development of insulin resistance and diabetic pathology.
AIM: The aim of this study was to evaluate the concentrations of individual adipocytokines and metabolic hormones in patients with DM2 and without diabetes, depending on the presence/absence of abdominal obesity (AO).
MATERIALS AND METHODS: A single-center observational cross-sectional study was conducted. A population subsample of men and women aged 25–44 years was examined. Socio-demographic data were collected, anthropometric measurements were performed. The levels of amylin, C-peptide, ghrelin, glucose-dependent insulinotropic polypeptide, glucagon-like peptide 1 (GLP-1), glucagon, were determined in blood serum by multiplex analysis using a set of reagents Human Metabolic Hormone V3 (USA) and Human Adipokine Panel 1 (USA) on a Luminex MAGPIX flow fluorimeter (USA). interleukin 6, insulin, leptin, monocytic chemotactic factor 1 (MCP-1), pancreatic polypeptide (PP), peptide YY (PYY), tumor necrosis factor alpha (TNF-α), adiponectin, adipsin, lipocalin-2, plasminogen activator inhibitor-1 (PAI-1) and resistin.
RESULTS: The study included 105 people. The main group consisted of 35 people with diabetes mellitus, 11 of them without AO and 24 with AO, the control group consisted of 70 people without diabetes mellitus (35 people with AO and 35 without AO), comparable in gender and age with the main group. In individuals with abdominal obesity, regardless of the presence of type 2 diabetes mellitus, the levels of C-peptide, GLP-1, insulin, leptin and TNF-alpha are higher than in individuals without abdominal obesity. The chance of having diabetes mellitus and AO is associated with an increase in leptin levels (OR=1.367, 95% CI: 1.050–1.779, p=0.020).
CONCLUSION: The results of our study show that the indicators of the adipocytokine profile differ significantly in individuals with the presence/absence of abdominal obesity. According to our data, leptin makes the greatest contribution to the development of SD2 against the background of AO. Further research is needed to identify causal relationships and determine whether treatment that regulates adipocytokine levels can help in personalized approaches to the prevention and treatment of type 2 diabetes mellitus.
BACKGROUND: Excessive deposition of the epicardial adipose tissue (EAT) plays a role in the development of a number of cardiovascular diseases, including ischemic stroke. As more than half of strokes in patients with atrial fibrillation (AF) are cardioembolic, and the source of thromboembolic complications is the left atrial appendage (LAA), it can be assumed that excess EAT contributes to the development of LAA thrombus. The literature does not present the results of a study of the relationship between the amount of EAT and LAA thrombus in patients with AF, which makes it relevant to study this issue.
AIM: to study the effect of EAТ on LAA thrombosis and the emptying flow velocity from the LAA in patients with persistent AF.
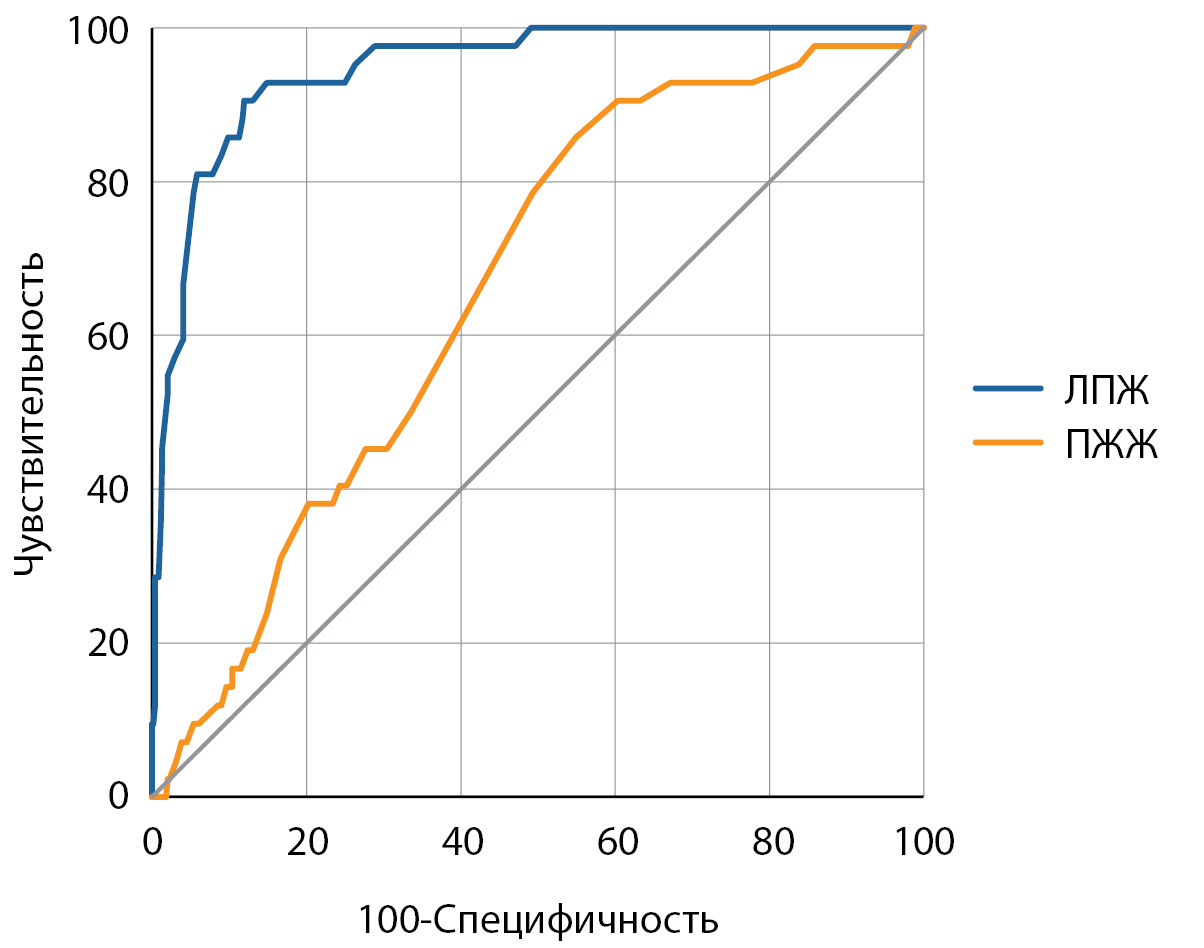
MATERIALS AND METHODS: The patients with persistent AF underwent transesophageal and transthoracic echocardiography before the planned cardioversion. The transesophageal echocardiography measured the emptying flow velocity from the LAA, and the thickness of the interatrial septum and the left lateral ridge, the average value of which was used to estimate the amount of left atrial EAT. The thickness of the anterior wall of the right ventricular EAT was measured by transthoracic echocardiography.
RESULTS: The LAA thrombus was detected in 42 (8.6%) patients of 486 patients with persistent AF (age 64.0 [59.0; 70.0] years, men 58.0%). Patients with thrombus had greater thickness of the left atrial EAT (9.30 [9.05; 9.55] vs. 7.70 [7.03; 8.28] mm, p<0.001) and of the right ventricular EAT (8.05 [7, 90; 8.90] versus 7.80 [7.20; 8.40] mm, p = 0.001), but the emptying flow velocity from the LAA is lower (20.0 [14.0; 26.0] versus 32.0 [26.0; 39.0] cm/s, p<0.001). Area under the receiver operator characteristic curve for the thickness of the left atrial EAT, as a predictor of the LAA thrombosis, was significantly larger than for the thickness of the right ventricular EAT: 0.947 (0.923–0.965) versus 0.661 (0.617–0.703), p<0.001. The thickness of the left atrial EAT more than 8.6 mm increases the chances of LAA thrombosis by 70.1 (24.1–204.2) times. Analysis of multiple linear regression did not reveal an independent effect of the thickness of the left atrial EAT (b = -0.0951±0.6163, p = 0.877) and of the right ventricular EAT (b = 0.6764±0.4383, p = 0.124) on the emptying flow velocity from the LAA.
CONCLUSION: The increased of the thickness of EAT increases the chances of developing LAA thrombosis in patients with persistent AF, but does not affect on the emptying flow velocity from the LAA.
BACKGROUND: A special role in the development of obesity is given to the genetic polymorphism of lipid metabolism enzymes, which include triacylglycerol lipase. However, there is still no information about the relationship between the single nucleotide polymorphism (snp) of the triacylglycerol lipase (LIPC) gene and the state of the endocrine function of mesenchymal tissues in childhood and adolescence obesity.
AIM: The aim of the work was to study the relationship between snp LIPC for rs2070895 and changes in the content of adipokines, myokines, and the values of blood lipid metabolism in obese children and adolescents with different sexes.
MATERIALS AND METHODS: In 96 healthy children and adolescents of different sexes and 98 obese peers, a study was conducted to assess the snp of the LIPC by rs2070895. In the blood serum of the examined, the content of total cholesterol, HDL cholesterol, LDL cholesterol, VLDL cholesterol, triacylglycerols, glucose, activity of alanine aminotransferase and aspartate aminotransferase, as well as the level of leptin, adiponectin, resistin, apelin, irisin, adipsin, myostatin, FGF21, osteocrine, oncostatin M , insulin and asprosin.
RESULTS AND DISCUSSION: It has been established that obesity in boys is accompanied by hyperleptinemia, the occurrence of insulin resistance and disorders of blood lipid metabolism. In carriers of the heterozygous allele -250G/A, dyslipidemia and atherogenesis decrease in obesity, but alteration of internal organs increases. In girls with different LIPC genotypes for rs2070895, with obesity, there is an increase in the level of leptin and apelin, as well as irisin and insulin in the blood. In girls with the homozygous allele -250G/G, in addition to that, the content of resistin, asprosin and prolactin decreases in the blood, which is not are typical for girls with the heterozygous allele -250G/A. In obese girls with the heterozygous allele, the levels of adipsin, FGF-21, oncostatin M, and osteocrine increase, which are not typical for obese girls with the homozygous allele. Against the background of changes in the content of adipokines and myokines in girls homozygous for LIPC, obesity occurs dyslipemia, which is not typical for girls with the heterozygous allele -250G/A.
CONCLUSION: The snp of LIPC at rs2070895 has sex-dependent effects on the levels of adipokines, myokines, and parameters lipid metabolism in the blood.
BACKGROUND: Overweight and obesity have a significant impact on the course and results of treatment of many diseases, including cancer. One of the modern types of antitumor therapy is immune checkpoint inhibitors. Taking into account the high effectiveness of immune checkpoint inhibitors for various types of tumors, it seems interesting to study the initial anthropometric data of patients and assess the possible influence of nutritional status on the development of endocrine immune-mediated adverse events.
AIM: To compare groups of patients with different starting body mass index (BMI) before the first administration of the immune checkpoint inhibitors drug and analyze the risk of developing endocrine immune-mediated adverse events in the future.
MATERIALS AND METHODS: The single-center study included 172 patients who were recommended antitumor therapy immune checkpoint inhibitors at the N.N. Blokhin National Medical Research Center of Oncology and Moscow City Oncology Hospital №62 in 2020–2022. Measurement of height and body weight with further calculation of BMI was carried out before the first administration of the drug immune checkpoint inhibitors.
Depending on the subsequent occurrence of immune-mediated adverse events, patients were divided into groups: those with developed immune-mediated adverse events (any, cutaneous, thyroid) and those without immune-mediated adverse events (any, cutaneous, thyroid).
RESULTS: According to the results of our study, in 38 patients (37.3%) out of 102, for whom data on the presence/absence of any immune-mediated adverse events were obtained, the following were recorded: thyropathies (n=13, 12.7%), skin lesions (n=13, 12.7%), gastrointestinal toxicity (n=7, 6.9%), hepatotoxicity (n=4, 3.9%), hypophysitis (n=2, 2%), nephritis (n=2, 2%), diabetes mellitus (DM) (n=1, 1%), hematological toxicity (n=1, 1%), pneumonitis (n=1, 1%), Guillain-Barré syndrome (n=1, 1%). At the same time, in most patients only one immune-mediated adverse event was encountered (n=31, 81.6%), two immune-mediated adverse events were detected significantly less frequently (n=7, 18.4%).
When conducting a comparative analysis of groups of patients with developed immune-mediated adverse events, including dermatological ones, or their absence, a statistical trend in differences in BMI was obtained. Using ROC analysis, a BMI cut-off point was determined equal to 28.16 kg/m² for all immune-mediated adverse events and 25.39 kg/m² for skin immune-mediated adverse events, below which, contrary to the available data, the risk of developing immune-mediated adverse events increased, but the diagnostic sensitivity (DS) and diagnostic specificity (DS) turned out to be low.
CONCLUSION: We identified a statistical trend in the risk of developing immune-mediated adverse events (primarily dermatological) with a lower BMI before the start of antitumor immunotherapy immune checkpoint inhibitors. More research is required to find a more reliable relationship.
REVIEWS
The prevalence of obesity and type 2 diabetes continues to grow, which determines the need to develop new methods of prevention in order to reduce the population risks of developing these diseases. The current direction is to limit the consumption of easily digestible carbohydrates and use low-calorie or non-calorie sweeteners instead. Currently, there is an increase in the use of non-calorie sweeteners in the manufacture of food. In this regard, the study of their possible effects on metabolic processes is of great importance.
This review presents studies that have shown different effects of non-calorie sweeteners on carbohydrate and fat metabolism, body weight, the composition of intestinal microbiota, as well as the regulation of eating behavior. Some studies show that low-calorie sugar substitutes can be used in obese people as part of a comprehensive weight loss program, as well as in patients with type 2 diabetes mellitus with the aim of reducing postprandial hyperglycemia. Other studies demonstrate the negative effect of a number of low-calorie sweeteners on carbohydrate metabolism.
The main search for materials was carried out in Pubmed databases, eLIBRARY.ru, Google Scholar. Temporary search criteria 2012–2023 The relevant additional literature was included after a manual search in the literature lists of the included articles.
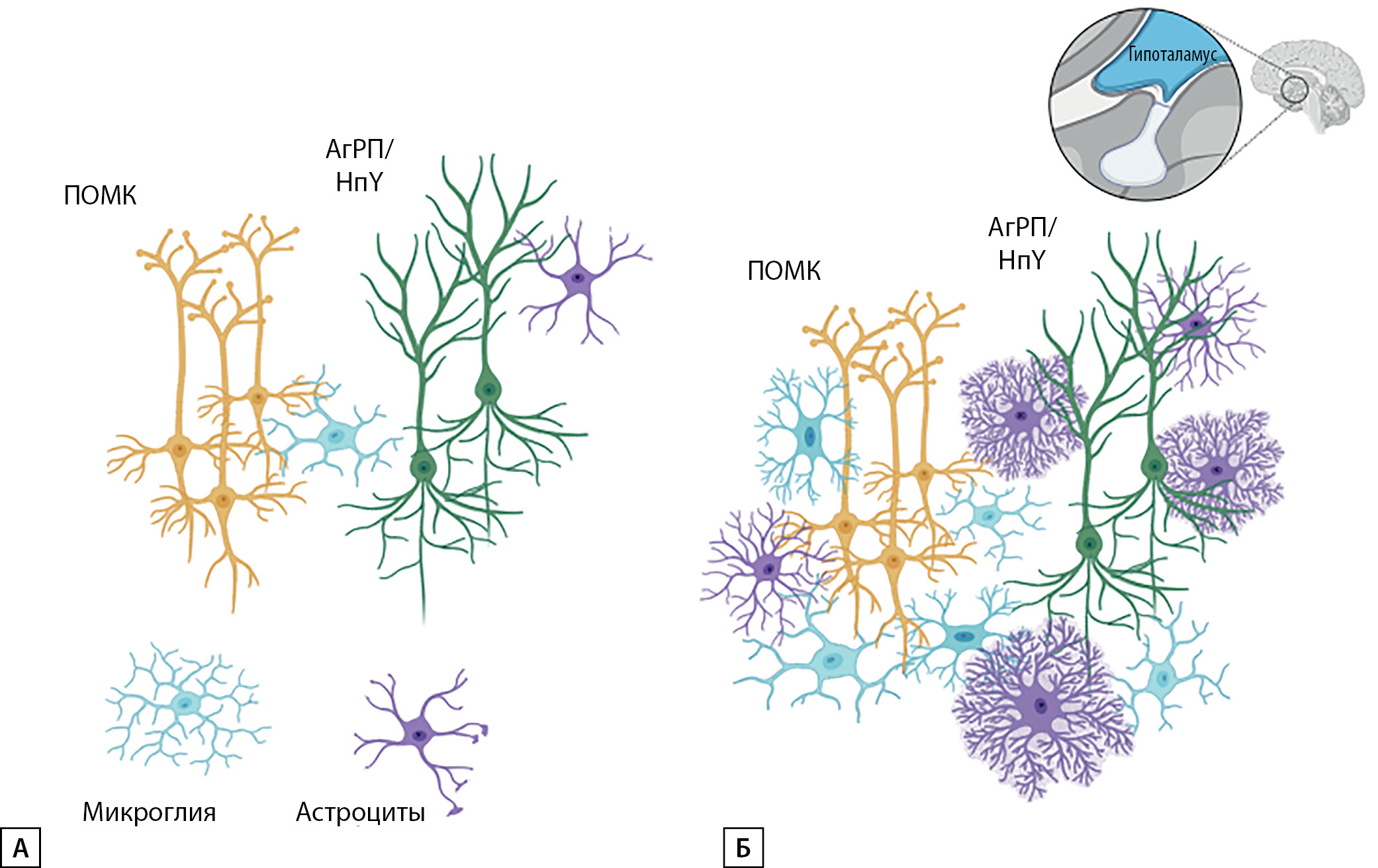
The article discusses certain aspects of the relationship between neurological diseases and metabolic disorders that are extremely relevant in connection with the pandemic spread of obesity. The pathogenesis of damage to the nervous system (NS) is considered in detail. The influence of the main metabolic factors on the development of cerebrovascular diseases (CVD), incl. neuroinflammation, changes in hemostasis, etc. is demonstrated. The problem of the development of cognitive dysfunction against the background of obesity due to the formation of atrophic processes in brain structures is highlighted. Modern possibilities of evaluation and modulation of eating behavior due to brain stimulation using functional magnetic resonance imaging (fMRI) and navigational rhythmic transcranial magnetic stimulation (rTMS) are described.
The problem of cerebrometabolic health is presented as a continuum of metabolic and cerebral disturbances. The mechanisms of interaction between the two most important systems of the body allow us to consider the changes that occur in them as an integral neuroendocrine alteration.
CASE REPORTS
Multiple endocrine neoplasia type 1 (MEN1) and congenital adrenal hyperplasia (CAH) are rare monogenic hereditary endocrinopathies with a prevalence of 1–9 cases per 100,000 and 9–15 cases per 100,000, respectively. MEN1 is characterized by the development of multiple endocrine and nonendocrine organ tumors, including parathyroid, pituitary, and duodenopancreatic neuroendocrine tumors (NETs), which constitute the classical triad of the disease. CAH is associated with genetic defects in enzymes and transport proteins involved in the synthesis of adrenal cortical steroid hormones. Overall, cases of the combination of two hereditary diseases in one patient are extremely rare. In this article, we describe a clinical case of the combination of MEN-1 with all three classical components and CAH, which, taking into account the low prevalence of both diseases, represents scientific interest. To date, only one similar case has been described in the literature. In addition, the paper discusses the pathogenetically determined combination of CAH and Ehlers-Danlos syndrome, known as the CAH-X syndrome.
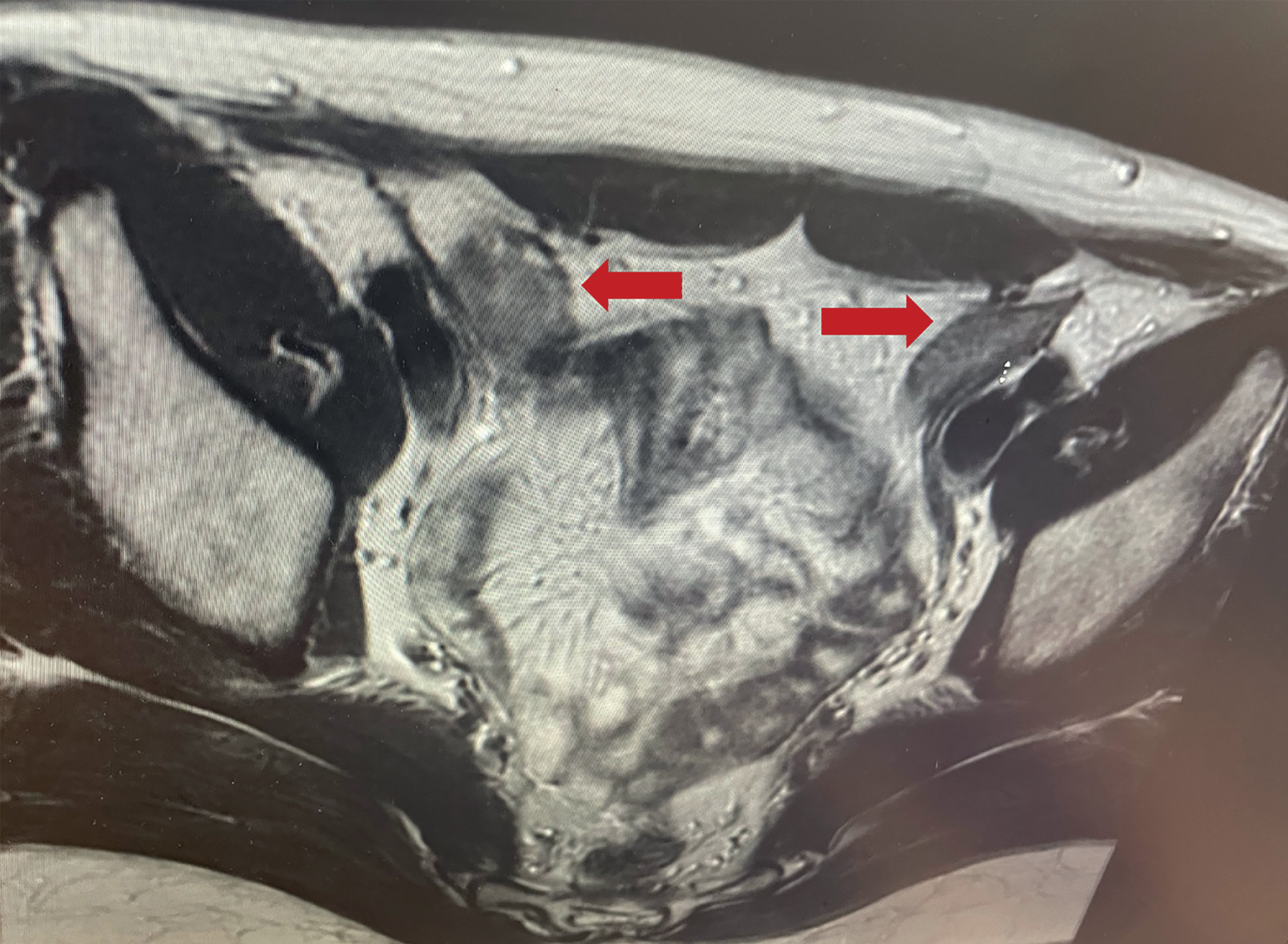
Androgen insensitivity syndrome is a genetic disorder characterized by complete or partial androgen insensitivity in individuals with a 46XY genotype. It is also the most common cause of disorders of sexual differentiation in patients with a 46XY karyotype. This condition is caused by a defect in the androgen receptor gene (AR), leading to abnormal development of male genitalia, impaired formation of male secondary sexual characteristics, and phenotypic features resembling the female sex.
One of the important aspects related to the management of androgen insensitivity syndrome is the necessity of preventive gonadectomy. However, the rationale for prophylactic removal of gonads remains a subject of debate. This article presents a clinical case of a 37-year-old woman with complete androgen insensitivity syndrome who, despite recommendations for gonadectomy based on suspicious MRI characteristics of the gonads, made the decision to decline surgical intervention, justifying her choice by the positive impact of gonadal hormonal activity on her external appearance and physical characteristics. This clinical case highlights the complexity of decision-making in the management of androgen insensitivity syndrome, where patient preferences and needs may play a significant role, despite potential risks and concerns surrounding the preservation of gonads.
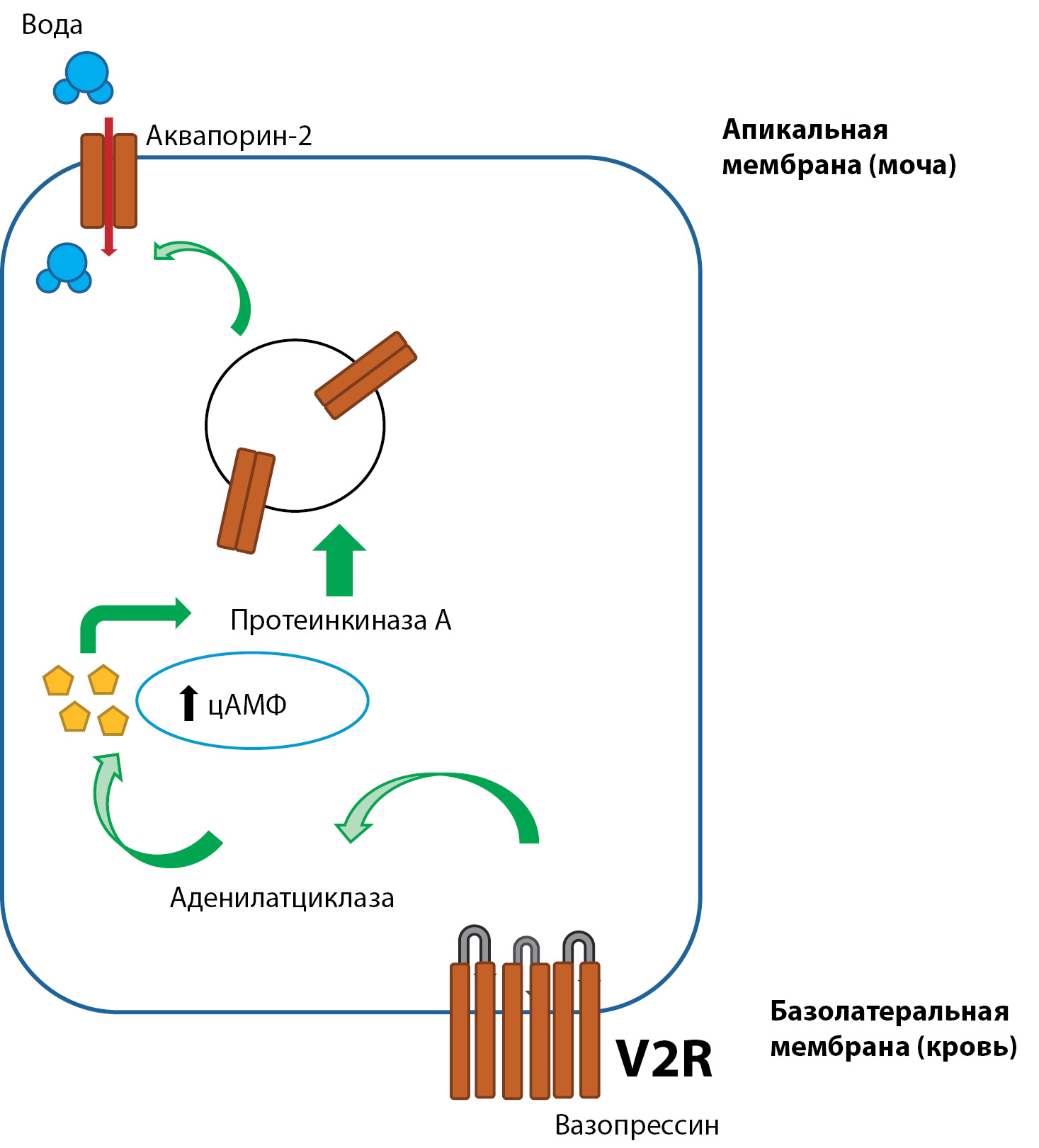
Nephrogenic diabetes insipidus is a heterogeneous disease in the etiopathogenesis of which are involved acquired and congenital factors. In this case, the kidneys do not respond to vasopressin and continue to produce large concentrated volumes of urine. Distinctive features in the pathology of central genesis are the fact of trauma, brain tumor with involvement of pituitary gland, response to intranasal vasopressin in the form of decreased diuresis.
For diagnosis it is important to perform a series of differential diagnostic tests.
In this article we present a unique clinical case of a patient with a long-term course of diabetes insipidus with the development a spectrum of comorbid conditions, metabolic disorders, required kidney transplantation.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2306-5524 (Online)