REVIEWS
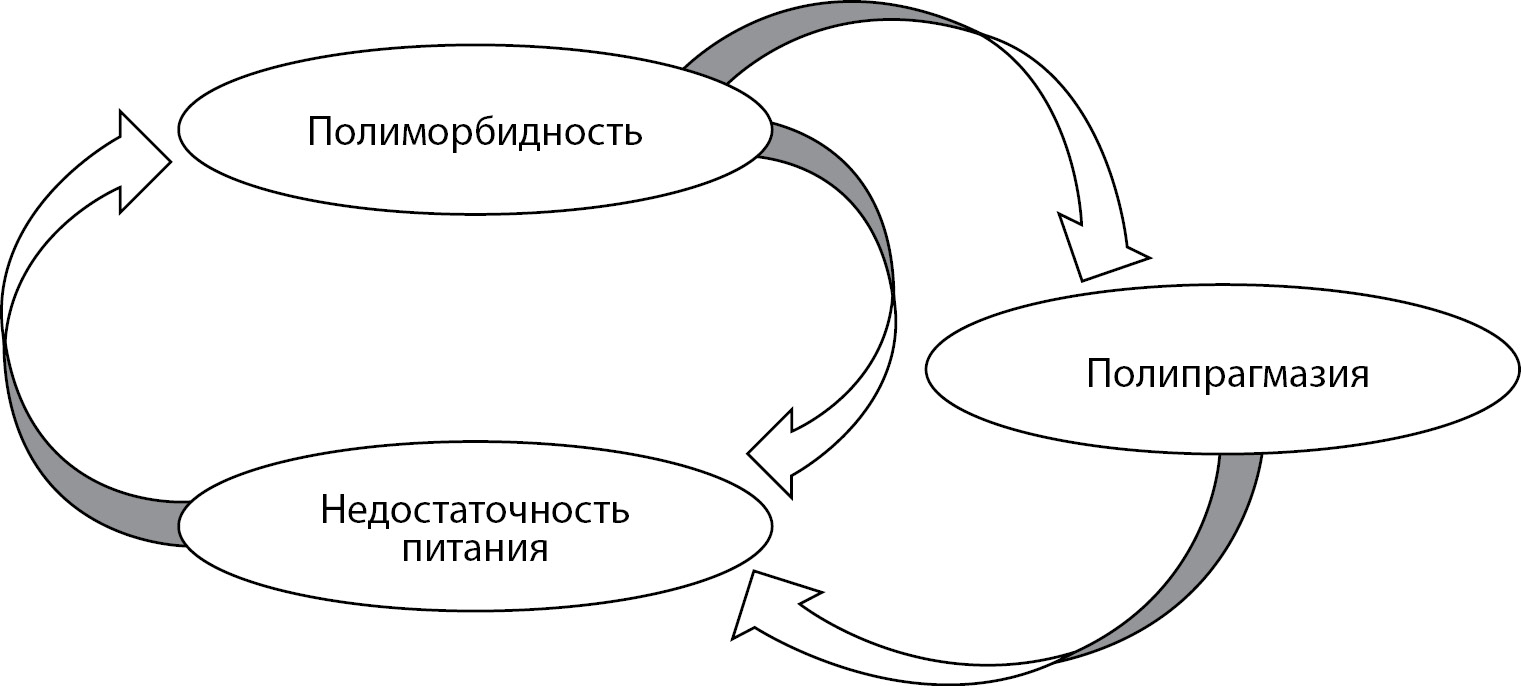
Increasing life expectancy and, as a consequence, a large number of comorbidities lead to a multitude of medications prescribed by physicians of different specialties. Patients with obesity and carbohydrate metabolism disorders, especially with type 2 diabetes mellitus (DM2), are at particular risk of polypragmasy, which is associated with the use of potentially nonrecommended medications. Prescribing errors can cause significant harm to the patient’s health and increase the risk of rehospitalization and healthcare costs. Identification of probably not recommended drugs in this category of patients will improve understanding of prevalence and risk factors of their use, develop strategies to prevent and limit the burden of taking inappropriate drugs and promote development of personalized and patient-oriented treatment options. Tools exist to assess potentially inappropriate therapy (PIT) in the elderly and new tools and criteria are often created. However, they are not specifically aimed at people with obesity and carbohydrate metabolism disorders. Thus, these criteria usually include only a few items related to DM2. Consequently, there is a clear need for a modern tool that can be used to address PIT specifically in older adults with obesity and carbohydrate metabolism disorders.
Diabetic nephropathy (DN) is a specific kidney involvement in diabetes mellitus (DM), caused by hemodynamic and metabolic factors. In the kidneys takes place an important step in the metabolism of vitamin D — 1α-hydroxylation, which results in the formation of its biologically active form. Reduced number of functioning nephrons in DN leads to impaired vitamin D metabolism, contributing to the development of a number of complications. In this review, we have focused in detail on both normal vitamin D metabolism and the features of vitamin D metabolism in chronic kidney disease (CKD). DN is the most common cause of CKD and, as a consequence, of kidney transplantation and one of the leading causes of cardiovascular morbidity and mortality in patients with DM. Bone mineral disorders resulting from abnormal vitamin D metabolism are also independent factors of high mortality among patients with DM. The final part of our review briefly highlights current approaches to vitamin D therapy in CKD and, in particular, in DN. It is worth noting that, despite the increasing number of patients with DN, there is currently no unified view on the use of vitamin D as a therapeutic agent in this pathology.
Currently, increasing evidence shows the mutual influence of aldosterone and adipose tissue. Aldosterone excess has been reported in patients with obesity and metabolic syndrome. Aldosterone has a direct effect on adipose tissue increasing anabolic activity and expression of mineralocorticoid receptors. In turn, excessive activation of MCR leads to stimulation of adipogenesis and an increase in the volume of adipose tissue. Aldosterone excess can be considered an independent cardiovascular risk factor that affects such processes as cardiac fibrosis, nephrosclerosis, and arteriosclerosis. There is convincing evidence of higher prevalence and severity of impaired glucose homeostasis and lipid metabolism disorders among patients with primary hyperaldosteronism. Similar pathological changes are also observed in patients with obesity and metabolic syndrome. This review presents scientific data on the metabolic effects of aldosterone, in particular its effect on adipose tissue function, glucose and lipid metabolism. Treatment with mineralocorticoid receptor antagonists may provide substantial benefit in the management of metabolic syndrome, contribute to the stabilisation of glucose and lipid metabolism, improve clinical status of patients with cardiovascular diseases and reduce the risk of complications. However, available evidence from the conducted studies is not sufficient to justify introduction of such therapy into clinical practice.
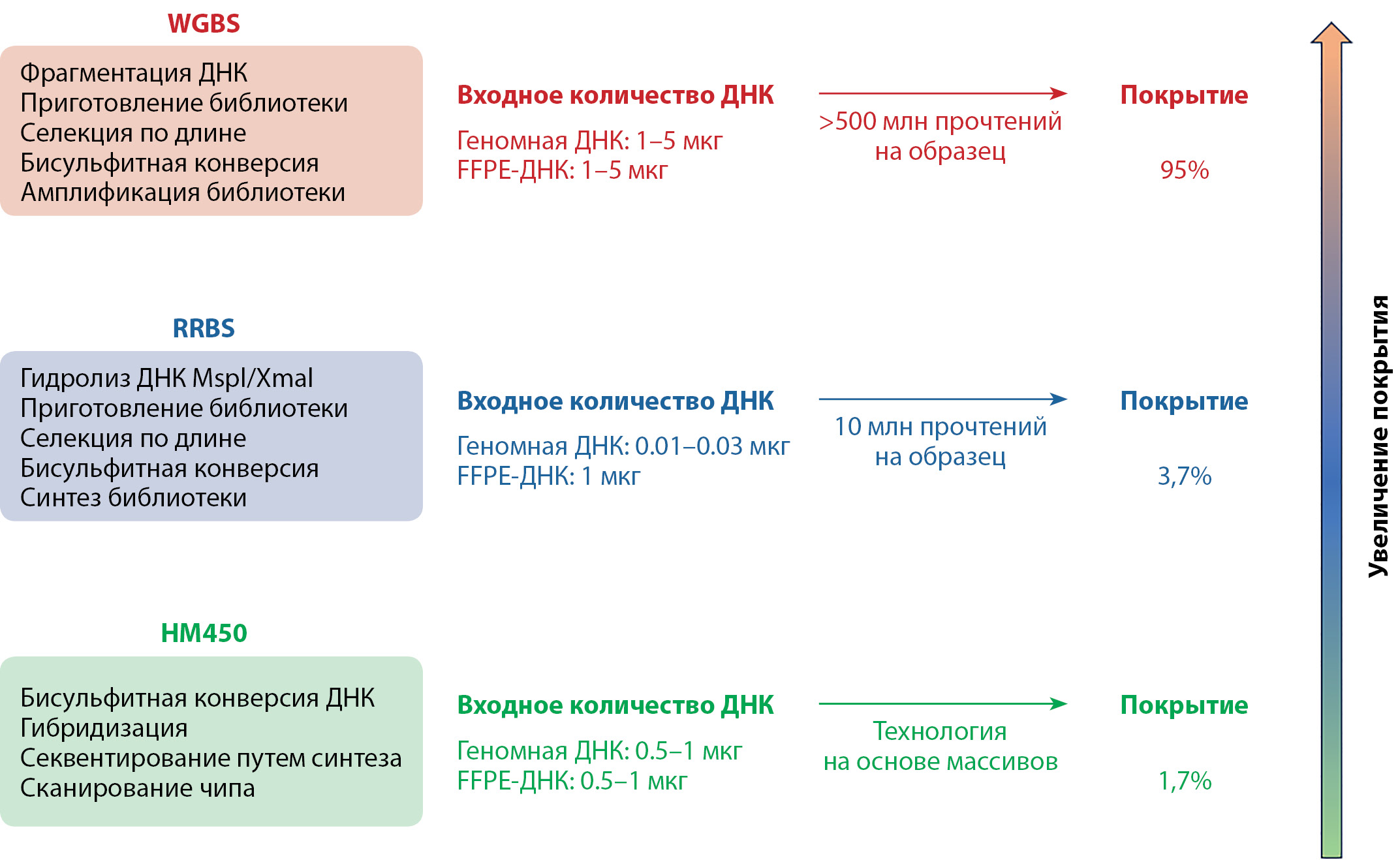
Obesity is a complex, heterogeneous, actively progressive disease manifested by excessive formation of adipose tissue in the body and usually has a high cardiometabolic risk and specific complications. Currently, new data are emerging that explain the pathogenesis of obesity not only by genetic variations and imbalance between energy intake and expenditure, but also by the influence of epigenetic mechanisms, such as DNA methylation. DNA methylation is the most studied epigenetic modification, whose status in the cell can be altered by various external and internal environmental factors, including diet, lifestyle, and hormones. These changes may lead to dysregulation of genes responsible for metabolic processes associated with the development of obesity. However, studies investigating epigenetic marks as potential mediators of obesity are heterogeneous in design, methodology, and results. This review discusses a conceptual framework analyzing the relationship between DNA methylation, obesity, inflammation, and response to weight loss, including after bariatric surgery, as well as material selection and methodology issues to consider when designing studies in this area.
ORIGINAL STUDIES
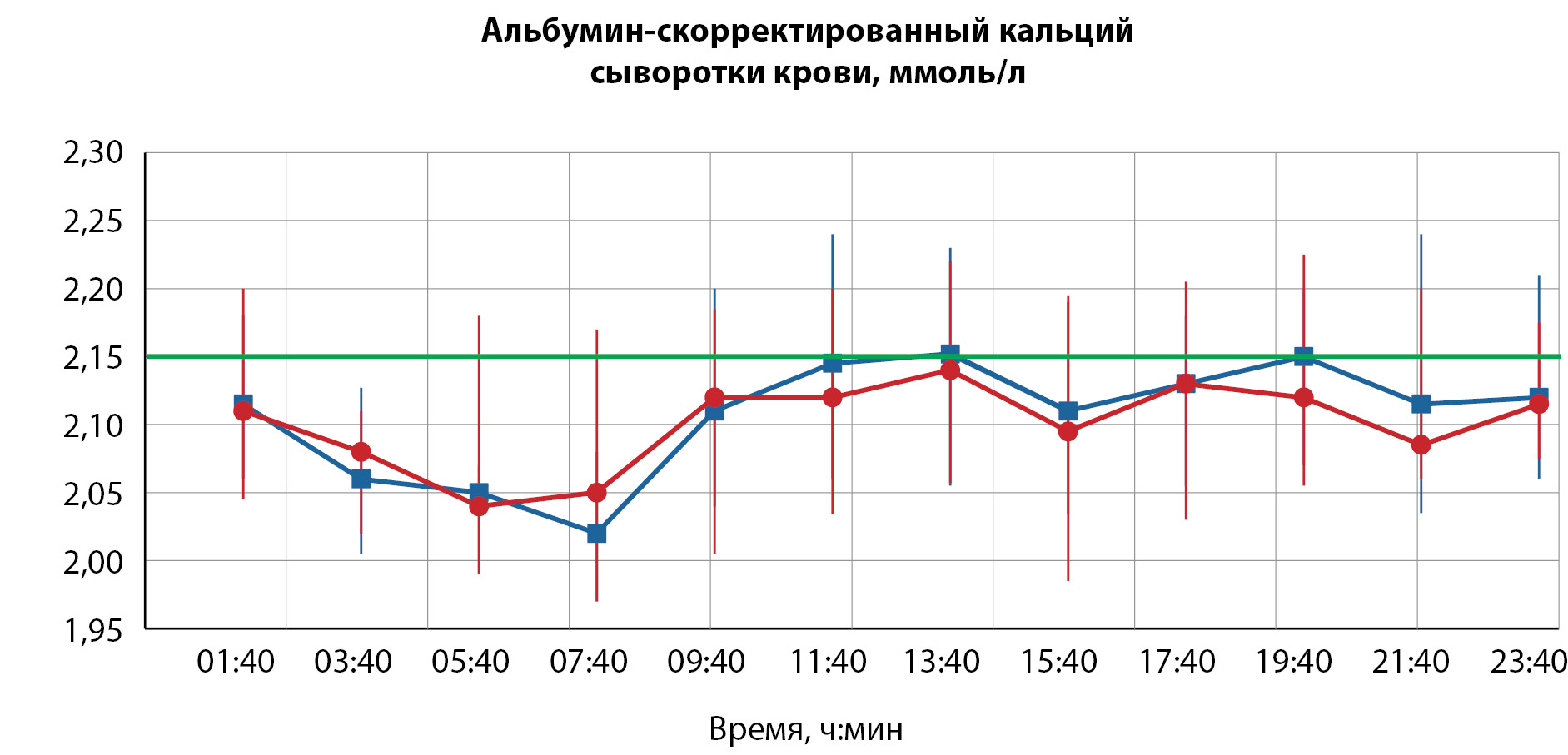
BACKGROUND: Chronic hypoparathyroidism is a relatively rare disease, which usually treated active forms of vitamin D and oral calcium supplements. Supplementation with native vitamin D can be useful both for achieving «non-skeletal» effects of vitamin D and for a more stable serum calcium profile.
AIM: The aim of this study was to estimate the daily serum calcium and 24-hour urine calcium levels depending on different 25(OH) vitamin D values in patients with chronic hypoparathyroidism on treatment of active forms of vitamin D and calcium supplements.
MATERIALS AND METHODS: Forty patients with chronic hypoparathyroidism were involved in the study. All patients were divided in two groups, matched on sex and age, according to the median level of 25(OH) vitamin D in the total group.
RESULTS: There were no significant differences between groups by total, albumin-adjusted serum calcium levels and urine calcium excretion. Patients with serum 25(ОН) vitamin D level ≥ 35 ng/ml had significant tendency to achieve more often the target levels of total serum calcium during the day (128 vs. 149 measurements during the day, p=0.049, χ2). However, this tendency disappeared for albumin-adjusted serum calcium levels (p=0.517, χ2). There frequency of hypercalcemia by albumin-adjusted serum calcium in the group of patients with 25(ОН) vitamin D ≥ 35 ng/ml (p=0.006, χ2) was significantly lower, but not for total serum calcium (a trend, p=0.042, χ2). As regards hypocalcemia, there were no significant differences by albumin-adjusted serum calcium (p=0.581, χ2) and it tends to lower frequency by total serum calcium (p=0.023, χ2).
CONCLUSION: The additional administration of native vitamin D in patients with chronic hypoparathyroidism may have some advantages, related to the general concept of worldwide vitamin D deficiency and better disease control.
BACKGROUND: Pituitary adenomas are the third most common intracranial neoplasm. Clinical significance is determined by the nature of growth and hormonal activity, leading to disruption of various parts of metabolism. Medical registries are a valuable tool for assessing clinical and epidemiological parameters and obtaining data on real-life clinical practice.
AIM: To analyze the epidemiological and clinical characteristics of four pituitary disorders in Russian Hypothalamic and Pituitary Tumor Registry (OGGO): acromegaly, Cushing’s disease, prolactin-secreting and non-functioning pituitary adenomas
MATERIALS AND METHODS: The object of the study is the database of the OGGO registry, which includes 84 regions of the Russian Federation, as of 01/01/2023.
RESULTS: The maximum prevalence of acromegaly in the Russian Federation was noted in Karelia (9.48/100 thousand) and Chuvash Republic (10.8/100 thousand) and in Tyumen region (8.9/100 thousand). The incidence of acromegaly in 2021 was 0.6/1 million population. The maximum prevalence of Cushing’s disease is observed in Karelia Republic (2.33/100 thousand), Chukotka (2.01/100 thousand), Kirov (1.79/100 thousand) and Tver region ( 1.79/100 thousand). The incidence of Cushing’s disease in 2021 was 0.1/1 million population. The maximum prevalence of prolactinomas is observed Karelia (13.33/100 thousand) and Chuvash Republic (12.35/100 thousand) and in Voronezh region (8.66/100 thousand). The incidence of prolactin-secreting adenomas in 2021 was 0.6/1 million population. The maximum prevalence of non-functioning pituitary adenomas is observed in the Karelia (15.08/100 thousand), Voronezh region (8.82/100 thousand), Tyumen region (8.11/100 thousand) and Sakha/Yakutia Republic (7.56 /100 thousand). The incidence of non-functioning pituitary adenomas in 2021 was 0.3/1 million population. The median age for acromegaly was 63.6 [53.2;71.5], for Cushing’s disease 49.2 [38.8;60.8], for prolactin-secreting adenomas 47.5 [38.3;59.7], for patients with non-functioning pituitary adenomas — 58.4 [43.8;67.9] . At the time of the last visit, remission was observed in 42.7% of patients with acromegaly, 62.5% with Cushing’s disease, 39.7% with prolactinomas and 76.6% of patients with non-active adenomas.
CONCLUSION: The OGGO registry is a valuable tool for assessing epidemiological, clinical data and treatments used. At the same time, the quality of the analysis directly depends on the quality and completeness of the entered data. Further research in the field of epidemiology of endocrinopathies should be aimed at improving the quality and ease of data entry, which will allow obtaining the most complete patient characterization.
BACKGROUND: dyslipidemia is currently considered to be one of cardiovascular risk factors. Angiotensin II receptor type I (AGTR1) genetic polymorphisms are known as candidate genes for hypertension, diabetes, as well as for diabetes and obesity complications. Until now, there are not much data on how 1166A>C (rs5186) polymorphism of the AGTR1 gene correlates with Northerners’ carbohydrate and lipid metabolism disorders. In addition, the data are contradictory. Following on from this, we see it is relevant to study the subject.
AIM: this research assessed variants of 1166A>C (rs5186) polymorphism of the AGTR1 gene as a predictor of dyslipidemia, carbohydrate metabolism disorders, overweight, and hypertension.
MATERIALS AND METHODS: the North residents from Magadan Region, Caucasian by ethnicity, aged from 24 to 56 (average age 43.7± 1.4 yrs) participated in the survey. By real-time polymerase chain reaction we determined the single nucleotide polymorphism of the AGTR1 (rs5186) gene. We also analyzed physical development and cardiovascular variables as well as the concentrations of glucose, insulin, glycosylated hemoglobin, C-reactive protein, total cholesterol, triglycerides, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol. The insulin resistance index and the atherogenicity coefficient were calculated using standard methods.
RESULTS: the examined subjects were one hundred and one volunteers. According to the results of genetic analysis, 55 people were assigned to the group of homozygotes for the wild type (AA) and 46 people were assigned to the group of the AGTR1*C allele variant carriers (heterozygotes and homozygotes AC+CC). Our findings contributed to the evidence on more unfavorable lipid pictures showed by the AGTR1*C allele variant carriers: significantly high values of total cholesterol (5,77±0,11, р=0.045), low-density lipoproteins (3,87±0,09, р=0.009), triglycerides (1,43±0,06, р=0.035), and atherogenicity coefficient (3,61±0,10, р=0.001), along with significantly low values of high-density lipoproteins (1,30±0,03, р=0,008). The above indicators were observed as opposed to significantly high fasting glycemia (5,74±0,14, р=0.006) and glycosylated hemoglobin (5,74±0,09, р=0.001) exhibited by the AA homozygotes subjects whose indices could be defined as the state of prediabetes. No intergroup differences were found in anthropometric or cardiovascular variables.
CONCLUSION: thus, we could see impairments in the lipid pictures of the AGTR1*С polymorphic variant carriers along with the optimization of carbohydrate metabolism and no effect on the blood pressure or anthropometric characteristics.
BACKGROUND: It is known that insulinoma in approximately 5% of cases is associated with multiple endocrine neoplasia type 1 syndrome (MEN1), in which the prognosis and management tactics of patients have been developed in detail. The diagnosis of MEN1 often does not require genetic confirmation, since the syndrome has a typical clinical picture. At the same time, a combination of this tumor with other hereditary syndromes is found in the literature, which are characterized by the presence of malignant neoplasms of various localizations, primary multiple lesions, hormonal and other disorders. Thus, it is relevant to search for the genetic causes that cause the development of insulinoma, in addition to MEN1.
AIM: to evaluate the frequency of detection of genetic causes of the development of insulin-producing tumors of the pancreas, in addition to MEN1; to analyze the phenotypic characteristics of patients with such tumors.
MATERIALS AND METHODS: Based on the analysis of literature for the period up to 2020, a panel has been developed that includes coding regions of 10 genes (MEN1, VHL, TSC1, TSC2, KRAS, YY1, CDKN2A, MLH1, ADCY1, CACNA2D2) involved in the development of insulinoma. In 32 patients diagnosed with insulinoma, verified by pathomorphological examination, with the absence of clinical and/or genetic data indicating MEN1 syndrome, a panel of genes was sequenced with subsequent analysis of the identified genetic variants and phenotypic data obtained from the medical records of patients. In one patient, an additional molecular genetic study of the «Endom» panel was performed, revealing genetic variants of coding regions of 377 genes associated with endocrine diseases.
RESULTS: In 8 patients (25%, 95% CI (11%; 43%)), 9 variants of mutations were identified that were not classified as benign, at that two mutations in the TSC2 gene were detected in one patient. Frequencies of genetic variants: TSC2 — 13%, 95% CI (4%; 29%), MEN1 — 6% (1%; 21%), MLH1 — 3% (0%;16%), CDKN2A/P16INK4A — 3% (0%;16%). When comparing patients with the identified mutation, with the exception of benign (n=8), and patients without mutation or with a benign mutation (n=24), there were no differences in the Grade (degree of differentiation), Ki67 proliferation index, frequency of concomitant tumors, burdened history, multiple pancreatic lesions or recurrence of insulinoma, however, patients with germinal mutation were found at the level of statistical trend to be younger at the manifestation of insulinoma and to have bigger tumors. In a patient who underwent an additional molecular genetic study using the new «Endome» panel, previously undescribed gene variants (APC and KIF1B) associated with various sporadic tumors, including endocrine ones, were identified.
CONCLUSION: A panel of 10 genes has been developed, mutations of which are associated with insulinoma. A relatively high incidence of genetically determined insulinoma was determined (25% of cases), in half of cases — against the background of tuberous sclerosis. We consider it relevant to evaluate the effectiveness of genetic testing for patients with insulinoma. We believe that, first of all, patients with a high risk of hereditary pathology should be examined: with the manifestation of the disease at a young age and with a large tumor. The identification of a genetic mutation will make it possible to determine the prognosis of the disease, optimize the monitoring algorithm in order to timely identify concomitant diseases-components of the hereditary syndrome, and conduct genetic counseling of the family.
CASE REPORTS
The relevance of developing an individual model of psychological support for patients with bariatric surgery «12 targets» in the framework of a multidisciplinary approach to the treatment of obesity is due to the fact that the effectiveness of surgical treatment is significantly influenced by the individual psychological characteristics of the patient. A comprehensive assessment of the psychological state of patients and the implementation of psychocorrective measures before and after bariatric surgery can improve the effectiveness of surgical treatment and prevent the risk of relapse. The individual model of the psychological support of the bariatric patient is built on the principle of a psycho-correction program, which is an integrative approach using psychotherapeutic tools from various areas of clinical psychology and psychotherapy. 12 universal targets of psycho-corrective influence in work with bariatric patients have been identified. The program is implemented in two stages: psychological preparation for bariatric surgery, psychological adaptation to physiological and psychological changes in the postoperative period. 20 bariatric patients took part in the program of individual psychological support, 11 of them (group 1) participated in all stages of psycho-corrective measures; 9 people (group 2) did not undergo psychological preparation for surgery, they were already included in the second stage of work on psychological adaptation to physiological and psychological changes in the postoperative period. Intermediate results of evaluating the effectiveness of psychological support for patients, which are based on the percentage of BMI reduction, show the achievement of stability in reducing overweight in the process of psychological interventions in both groups. The described model of psychological work will allow clinical psychologists working in a multidisciplinary team in bariatrics to focus on the universal targets of the problem field of a bariatric patient.
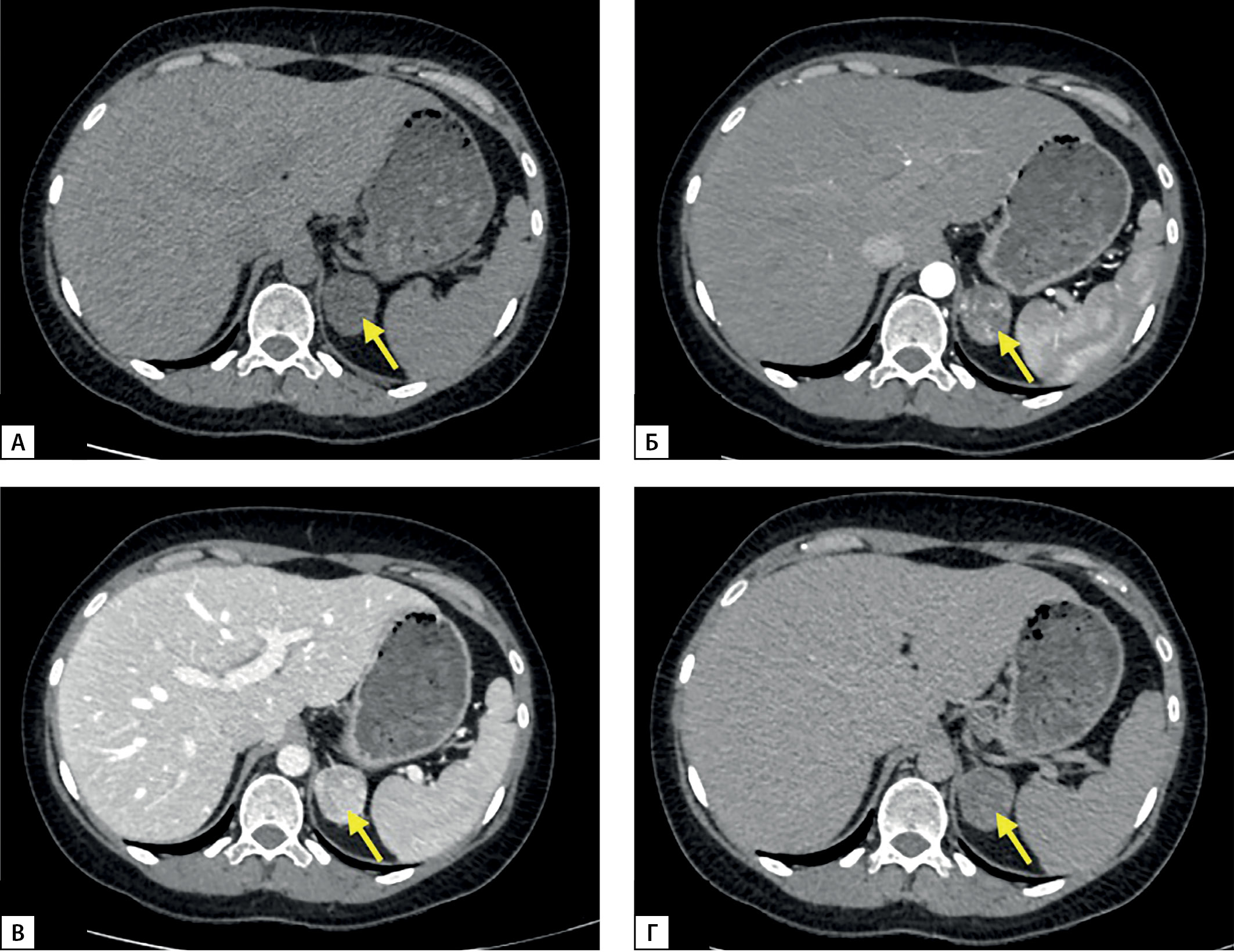
Hyperandrogenism is the most prevalent cause of menstrual cycle abnormalities and infertility in women. Here, we present a case of a 32-year-old woman with a 7-year history of menstrual irregularity and infertility. Laboratory test results revealed elevated 17-hydroxyprogesterone, progesterone 21-deoxycortisol. Abdominal computed tomography found a 3,9х2,9х2,6 cm left adrenal tumor. Non-classic congenital adrenal hyperplasia was diagnosed initially, however, treatment with supraphysiological doses of dexamethasone proved ineffective and progesterone and 17-hydroxyprogesterone levels remained high. Genetic testing revealed no 21-hydroxylase deficiency. Laparoscopic adrenalectomy was performed with subsequent pathological report being compatible with an adrenal cortical adenoma. 17-hydroxyprogesterone, progesterone 21-deoxycortisol levels returned to the normal range postoperatively and the patient’s menstrual cycle normalized without additional medication. Steroid metabolites producing adenomas are also extremely rare with only a few cases found in patients without previous CAH diagnosis. When a patient with clinically and biochemically diagnosed NCCAH demonstrate no typical features and shows poor response to steroid therapy, the patient should receive multisteroid LC–MS/MS assay for glucocorticoids and androgens, adrenal and ovarian imaging and undergo CYP21A2 gene mutation analysis.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2306-5524 (Online)