Case Report
Hyperpolactinemia is a persistent excess of prolactin in the blood serum. The symptom complex of hyperprolactinemia primarily consists of disturbances in function of the reproductive system. The secretion of prolactin is under complex neuroendocrine control, which involves factors of different nature: neurotransmitters, hormones of the peripheral endocrine glands. In most cases, prolactin is secreted by pituitary cells - lactotrophs, but in some cases, hypersecretion of prolactin is combined with an excess production of growth hormone, which is typical for tumors originating from the line of progenitor cells of lactotrophs and somatotrophs of the pituitary gland, mammosomatotrophs. In this case, the symptom complex of hyperprolactinemia is accompanied by clinical manifestations of acromegaly. In patients with acromegaly, the cause of hyperprolactinemia may be pituitary stalk compression or mixed secretion of prolactin and growth hormone. Differentiation of lactotropic and somatotropic pituitary cells is determined by transcription factor Pit-1. These cell lineages are closely connected, and this may be one of the reasons for formation of tumors with mixed secretion. Reports of late presentation of acromegaly in patients previously diagnosed with prolactinomas have also been described in literature.
Clinical manifestations of hyperprolactinemia can cause the patient to seek doctor’s attention before acromegalic changes in appearance develop. Careful attention is needed both to the primary diagnosis and to the clinical course of the disease in patients with hyperprolactinemia and pituitary adenoma: full assessment of hormonal status with mandatory evaluation of IGF-1 is crucial at initial examination, during further observation it may be advised to consider periodic evaluation of IGF-1 in addition to assessment of prolactin and the size of adenoma. Pituitary adenomas with mixed secretion may have a poorer prognosis.
Original paper
Background: The common pathogenetic relations of type 2 diabetes mellitus (T2DM), testosterone (T) deficiency and non-alcoholic fatty liver disease (NAFLD) have indicated a new direction in the study of their mutual influence. It was found that NAFLD is more pronounced in men with T2DM and hypogonadism than in eugonadal patients and associated with hyperinsulinemia, insulin resistance, impaired lipid metabolism and adipose tissue dysfunction. However, the effects of testosterone replacement therapy (TRT) on the severity of NAFLD in men with hypogonadism have not been studied.
Aims: To study the effect of TRT on the severity of NAFLD in men with T2DM and hypogonadism.
MATERIALS AND METHODS: Anthropometric data, biochemical parameters (alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyltranspeptidase (GGTP), glucose, immunoreactive insulin, HOMA index, glycosylated hemoglobin, lipidogram), ELISA analysis (total T, LH, sex hormone binding globulin, resistin, adiponectin, leptin), as well as magnetic resonance imaging with determination of the liver fat fraction were examined.
Results: The study included 60 men with T2DM and hypogonadism (mean age 54 [49; 57] years), who were randomized into 2 groups: 1 (n=30) - patients who received 1% transdermal T gel (50 mg/day) in addition to standard hypoglycemictherapy; 2 (n=30) - patients who received standard hypoglycemic therapy. The follow-up period was 6 months. T therapy was associated with a decrease in liver enzyme levels: AST by 31%, ALT by 21%, and GGTP by 15.9% (p<0.05) and the hepatic fat fraction by 1.7 times, which reflect the regress of liver inflammation, and, consequently, a decrease in the severity of NAFLD. Moreover, TRT has improved the function of adipose tissue - reduced the concentration of leptin by 1.4 times and resistin by 1.5 times, which was accompanied by an increase in adiponectin level by 1.3 times (p<0.01). The use of TRT was associated with decrease in the severity of visceral obesity, hyperinsulinemia by 1.5 times, an insulin resistance index HOMA by 2.2 times, fasting glycaemia and HbA1c levels, despite constant hypoglycemic therapy. Statistically significant decrease in the levels of total cholesterol and triglycerides was observed in men receiving TRT. Thus, a decrease in adipose tissue dysfunction and insulin resistance in men receiving TRT can be considered as a pathogenetic mechanism responsible for improving liver function and reducing the severity of NAFLD.
Conclusions: TRT in men with T2DM and hypogonadism is accompanied by regress of inflammatory activity in liver and intensity of hepatocytes steatosis, reflected by decrease in liver enzymes levels and liver fat fraction.
Background: Hypothalamic obesity often develops after surgical treatment of craniopharyngioma and is characterized by rapid weight gain, high frequency of metabolic disorders, body composition specificity and resistance to standard lifestyle modification approaches and medication therapy of obesity. Recent studies show that one of the mechanisms, explaining weight gain in these children is decrease in resting energy expenditure (REE).
Aims: To compare REE, body composition parameters, and the frequency of metabolic disorders in children with hypothalamic and simple obesity.
Materials and methods: The study included 60 obese children aged 7 to 17 years, divided into two groups. The study group included 20 children with hypothalamic obesity, developed after craniopharyngioma treatment. The control group consisted of 40 children with simple obesity. Body composition, REE, and metabolic disorders were associated in all children.
Results: Children with hypothalamic obesity showed a significant decrease of resting energy expenditure. The average decrease in REE was 13.1%, but in single patients it reached 33.4%. The percentage of fat mass in hypothalamic and simple obesity does not differ significantly (39.7% [36.2; 42.6] vs 38.8 % [35.9; 43.2]; p=0.69). Screening for metabolic disorders revealed a high prevalence of metabolic disorders in hypothalamic obesity: impaired glucose tolerance - in 10%; dyslipidemia - 55%, insulin resistance-50%, non-alcoholic fatty liver disease - 60 %.
Conclusions: Children with hypothalamic obesity showed a significant decrease of resting energy expenditure. When planning a diet in this group of patients it is preferable to use indirect calorimetry. Hypothalamic obesity even at an early age is associated with a high frequency of metabolic disturbance. Hypothalamic obesity in children is not associated with more pronounced hyperinsulinemia and insulin resistance compared to the simple obesity.
Background: Endothelial dysfunction is the first but reversible stage of atherosclerosis. A change in the functional state of the vascular endothelium, especially of a growing organism, can be the basis for the development of many diseases in adulthood. The study of the structural and functional state of peripheral vessels of adolescents with hypothalamic syndrome is extremely important for understanding of the mechanisms of formation of cardiometabolic risks.
Aims: to compare the structural and functional state of the vascular wall of young men with hypothalamic syndrome and constitutionally exogenous obesity.
Methods: During the study 360 males were examined (average age 21.27±2.44 years) and divided into 3 groups: group 1 -with hypothalamic syndrome (n=242); group 2 - with constitutionally exogenous obesity (n=98); control group - practically healthy individuals (n=20). Hypothalamic syndrome was verified in the presence of a symptom complex, including obesity and pink striae. Cross-group comparative analysis of results of clinical, laboratory and instrumental examination was carried out.
Results: In the group of patients with hypothalamic syndrome, endothelium-dependent vasodilatation (9.44±1.26 versus 10.37±1.21%; p=0.001) and endothelium-independent vasodilatation (10.29±1.28 versus 11.29±1.14%; p=0.001) is worse than in the group of patients with constitutionally exogenous obesity, and the rate of endothelium-dependent vasodilatation is lower than the generally accepted norm. In addition, among patients with hypothalamic syndrome, the stiffness of the vascular wall is higher than among patients with constitutionally exogenous obesity (15.47±2.58 versus 13.24±3.84%; p=0.001). Statistically significant correlations were revealed between the structural and functional state of peripheral arteries and hemodynamic, hormonal, metabolic changes, and the level of C-reactive protein (p<0.05).
Conclusions: The obtained data indicate a deterioration of endothelial function and an increase in vascular wall stiffness in obese patients, regardless of its etiology. The patients with hypothalamic syndrome have more pronounced structural and functional changes in the vascular wall are observed than patients with constitutionally exogenous obesity.
Background: Investigating the inflammatory status and iron metabolism in patients with impaired carbohydrate metabolism seems quite relevant, while only few studies are devoted to the relationship between metabolic parameters, including lipid profile, inflammatory status indicators and the state of ferrokinetics in diabetes mellitus types 1 and 2 in a comparative aspect.
Aims: To establish the direction of changes in the inflammatory status and the state of ferrokinetics in patients with type 1 and type 2 diabetes mellitus depending on lipid metabolism disorders.
Materials and methods: The study included 48 patients with type 1 diabetes, 81 patients with type 2 diabetes; 11 people with obesity without impaired carbohydrate metabolism made up the comparison group, 17 healthy volunteers - the control group. Low-grade inflammation was assessed by the levels of high-sensitive C-reactive protein (CRP), tumor necrosisfactor-а (TNF-а), ferritin, and erythrocyte sedimentation rate (ESR). The state of iron metabolism was evaluated by the main hematological parameters (hemoglobin, red blood cell count, hematocrit), serum iron concentrations, transferrin, ferritin and hepcidin concentrations. In all patients lipid metabolism parameters, glycated hemoglobin, and microalbuminuria were measured.
Results: Patients with type 1 and type 2 diabetes mellitus had significantly higher inflammatory markers concentrations-TNF-а, ESR, and CRP - in relation to obese patients without impaired carbohydrate metabolism and those in the control group. The highest production of TNF-а was observed in patients with type 1 diabetes mellitus (15.28 [12.41-24.41] pg/ml), whereas CRP (7.00 [3.00-11.85] ng/ml) and ESR (18.00 [9.00-27.00] mm/h) were higher in patients with type 2 diabetes. In the structure of the examined individuals with diabetes mellitus (regardless of its type), dyslipidemia type IIb in comparison with less atherogenic type IIa dyslipidemia was characterized by a higher production of CRP (6.9 [3.00-12.35] and 3.00 [1.80-8.70] ng/ml, respectively), ESR (20.00 [10.00-30.00] and 15.00 [5.00-24.50] mm/h, respectively) and ferritin (114.80 [48.90-196.45] and 50.90 [19.58-114.10] ng/ml, respectively). Compared to iron deficiency anemia, anemia of chronic diseases in diabetes mellitus patients was more often accompanied by dyslipidemia llb (χ2=2.743; p=0.098) and was characterized by a higher content of atherogenic fractions of cholesterol.
Conclusions: Patients with type 2 diabetes mellitus and a more atherogenic dyslipidemia profile (type IIb) have a phenotype of the local inflammatory mesenchymal reaction of the liver with an increase in acute-phase proteins predominantly of hepatic origin (CRP, ferritin), whereas individuals suffering from type 1 diabetes and less atherogenic lipid profile (type IIa) have a phenotype of an autoimmune, genetically determined inflammatory response. It has been established that anemia of chronic diseases developing in the background of diabetes mellitus is associated with a more atherogenic lipid profile, compared with iron deficiency anemia.
Background: mild hypocalcemia is a common laboratory finding that is not accompanied by the clinical symptoms. The most common causes of hypocalcemia are inadequate calcium intake and vitamin D deficiency. Given the high prevalence of vitamin D deficiency (insufficiency), it seems relevant to determine the daily variability of serum calcium levels before and after its supplementation.
Aims: to assess the effect of 25(OH) vitamin D level on the daily profile of serum calcium and 24-hour urinary calcium levels. MATERIALS AND METHODS: the interventional, prospective, comparative study of 10 healthy volunteers (women/men - 9/1) was performed. We have analyzed the daily profiles of serum calcium and 24-hour urinary calcium levels. Summary duration of this study was 8 months and consisted two hospitalizations. Statistical analysis was done on August 2020. The descriptive statistics are represented by medians and the first and third quartiles in Me (Q1; Q3), average, maximum, and minimum values M (min; max) and by absolute and relative frequencies.
Results: Me serum calcium levels (Catotaland Cacorr.) and 24-hour urinary calcium levels did not differ before and after vitamin D supplementation. However, the number of reference calcium values increased as 25 (OH) vitamin D level was reached more than 30 ng/ml from 90.8% to 100% for Catotal and from 94.2% to 97.5% for Cacorr. Episodes of hypocalcemia were registered in patients with low vitamin D levels: in 3.33% of cases according to Catotal and 5.8% for Cacorr. The frequency of hypocalcemia decreased for Catotal (to 0%) and for Cacorr. (to 2.5%) after treatment with cholecalciferol. Analysis of Catotal and Cacorr. deviations during the day showed a less variability of the calcium profile after treatment, This study also revealed circadian character of daily serum calcium profile with the presence of maximum (09:40-17:40) and minimum (23:40-07:40) values during the day.
Conclusions: Our study demonstrated the improvement of daily serum calcium profile after vitamin D supplementation. We confirmed the increased number of reference calcium values, decreased variability of serum calcium levels during the day and decreased frequency of hypocalcemia.
Review
The review analyzes the etiological and pathogenetic factors (including immunopathogenesis factors) of chronic obstructive pulmonary disease (COPD) and metabolic syndrome (MS), cites data on clinical and pathogenetic characteristics of combined pathology, emphasizes the commonality of risk factors and individual links of pathogenesis in syntropy.
The clinical and pathogenetic features of the comorbidity of COPD and MS are closely related to the severity of chronic “metabolic” inflammation induced by elements of adipose tissue. Functional and biochemical disorders recorded in metabolic syndrome (insulin resistance, hyperglycemia, dyslipidemia) are considered as factors contributing to dysfunction of the components of innate and adaptive immunity.
The review formulates a number of unresolved issues of the pathogenesis of comorbid pathology, the study of which is necessary to search for the mutual aggravating effect of COPD and MS mechanisms. In view of the clinical and laboratory metabolic syndrome equivalents variety, the authors emphasize the relevance of future studies of the pathogenetic features of chronic inflammation associated with the comorbidity of the main components of metabolic syndrome and COPD, to develop effective methods of prevention and pathogenetic therapy of comorbid pathology.
The gut microbiota affects the processes of food digestion, intestinal peristalsis, controls the work of the intestinal epithelium, has protective properties against pathogenic microorganisms, activating local immunity and stimulating the secretion of mucus by intestinal cells. Besides the gut microbiota participates in the metabolism of proteins, fats and carbohydrates, mediates the processes of gluconeogenesis, glycogenolysis, lipogenesis and lipolysis, and affects on feelings of hunger and satiety. All these processes occur because the gut microbiota produces active metabolites throughout their life activity. Gut microbiota and active metabolites of the gut microbiota activate the synthesis of hormones. The gut microbiota affects the synthesis of hormones such as glucagon-like peptide-1, glucagon-like peptide-2, YY-peptide, glucose-dependent insu-linotropic peptide, ghrelin, leptin, cholecystokinin, serotonin, and insulin. Disturbance of the secretion of these hormones is one of the links in the pathogenesis of endocrine diseases such as diabetes and obesity. Thus, the gut microbiota is an endocrine organ. Changes in the composition and functions of the gut microbiota lead to metabolic disorders.
This article describes the effect of gut germs and active metabolites of the gut microbiota on the synthesis hormones by means of receptor mechanisms, genes, and enzymes.
It is generally known that obesity increases the risk of developing cardiovascular disease. A pathological increase in the mass of adipose tissue leads to a violation of the control of lipid accumulation at the molecular level, abnormal lipid metabolism with the formation of metabolites, which are critical for the development of these pathologies against the background of obesity. Ceramides are one of these metabolites. Ceramides perform many physiological functions, but under pathological conditions they induce insulin resistance, uncouple cellular respiration and phosphorylation, activate cell apoptosis, and play an important role in the induction of adipose tissue dysfunction. Altering ceramide biosynthesis through dysregulation of key enzymes leads to the formation and accumulation of ceramides, which block insulin signaling and induce adipose tissue inflammation.
This review highlights the metabolism of ceramides, the reasons for their ectopic deposition in tissues in obesity, as well as potential intracellular signaling pathways that modulate ceramide activity.
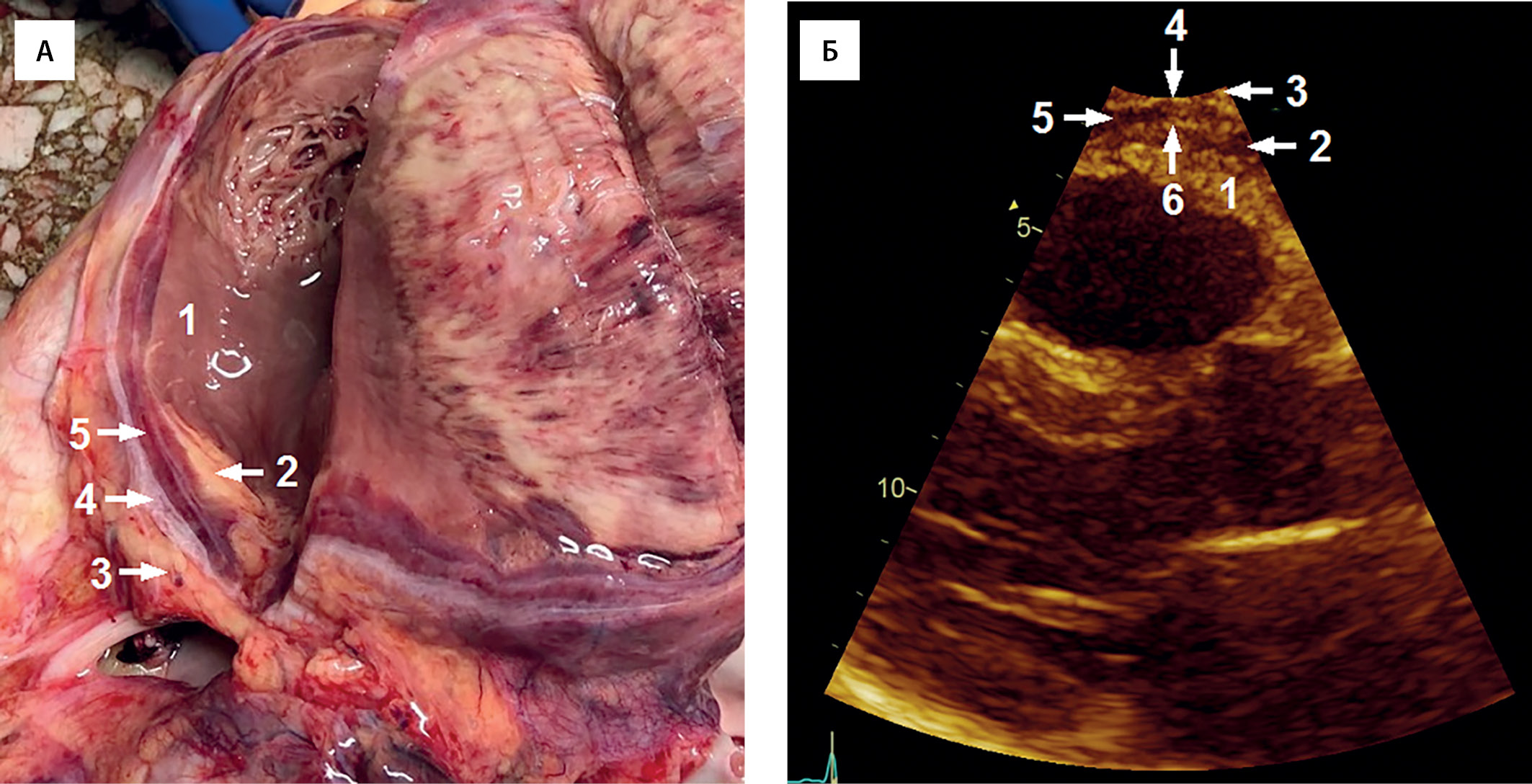
The studies, performed with MRI and CT, showed that the increase of fat, immediately adjacent to the myocardium (epicardial fat) is correlated more strongly with the risk of atrial fibrillation than the general or abdominal obesity. According to some studies, epicardial fat around the left atrium is a strong predictor of the development at atrial fibrillation. Also, the amount of the fat is associated with the effectiveness of cardioversion and the risk of developing thromboembolic stroke in patients with atrial fibrillation. The number of such works is small, since tomographic examinations are not needed if intra-atrial thrombosis is suspected, and transthoracic echocardiograthy does not allow visualization of atrial fat. However, transesophageal echocardiography is widely used in patients with atrial fibrillation and allows to measure the structures that serve as depots of epicardial fat, namely the interatrial septum and left lateral ridge. Accumulation of epicardial fat leads to thickening of these structures. This can be used to study the relationship between epicardial obesity and the risk of thromboembolic complications in patients with atrial fibrillations.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2306-5524 (Online)