ANNIVERSARY
ORIGINAL STUDIES
BACKGROUND: The people with an excessive amount of adipose tissue have elevated levels of free fatty acids (FFA) in the blood, which ultimately leads to disorders of lipid metabolism and insulin resistance, which are the main factors in the development of diabetes mellitus.
AIM: To study the content of FFA in blood plasma, as well as their association with body weight in men.
MATERIALS AND METHODS: A single-center observational one-stage study was conducted. The sample was formed by a random representative method, comparable by sex and age. The levels of FFA were determined in the blood plasma by high-performance liquid chromatography with mass spectrometry.
RESULTS: The study included 250 men. The selected participants were divided into groups according to their body mass index (BMI): Group 1 — 62 people with BMI≤24.9 kg/m2, Group 2 — 101 people with BMI 25.0–29.9 kg/m2, Group 3 — 87 people with BMI≥30.0 kg/m2. Obese men were divided into: Group 4 — 62 people with BMI 30.0–34.9 kg/m2, Group 5 — 19 people with BMI 35.0–39.9 kg/m2, Group 6 — 6 people with BMI≥40.0 kg/m2.
The content of docosatetraenoic acid was higher in groups 2 (p=0.002) and 5 (p=0.003), when compared with group 1. The content of gamma-linolenic acid was higher in group 3 than in group 1 (p=0.041). Concentration of oleic; linoleic; dihomo-gamma-linolenic; midic; arachidonic; eicosapentaenoic acids were higher in group 5 than in group 1 (p=0.007, p=0.023, p=0.004, p=0.019, p=0.006, p=0.001, respectively), and also than in group 2 (p=0.006, p=0.017, p=0.007, p=0.007, p=0.008, p=0.001, respectively). The content of nervonic acid is higher in groups 1 (p=0.029) and 2 (p=0.012) than in group 4. Obesity is associated with increased levels of gamma-linolenic (1.030, 1.006–1.056, p=0.015) and eicosapentaenoic acids (1.061, 1.000–1.125, p=0.045), and a decrease in the level of nervonic acid (0.953, 0.913–0.994, p=0.027).
CONCLUSION: The FFA levels of blood plasma is significantly different in men with normal body weight and the presence of obesity. The content of oleic, gamma-linolenic, midic, digomo-gamma-linolenic, arachidonic, docosatetraenoic and eicosapentaenoic acids was significantly higher in men with grade 2 obesity. An increase in the level of gamma-linolenic and eicosapentaenoic acids, and a decrease in the level of nervonic acid are associated with obesity, regardless of the age.
AIM: To determine the value of urine osmolality when conducting a test with 3% hypertonic sodium chloride solution, which allows for the differential diagnosis of diabetes insipidus (DI) and primary polydipsia (PP).
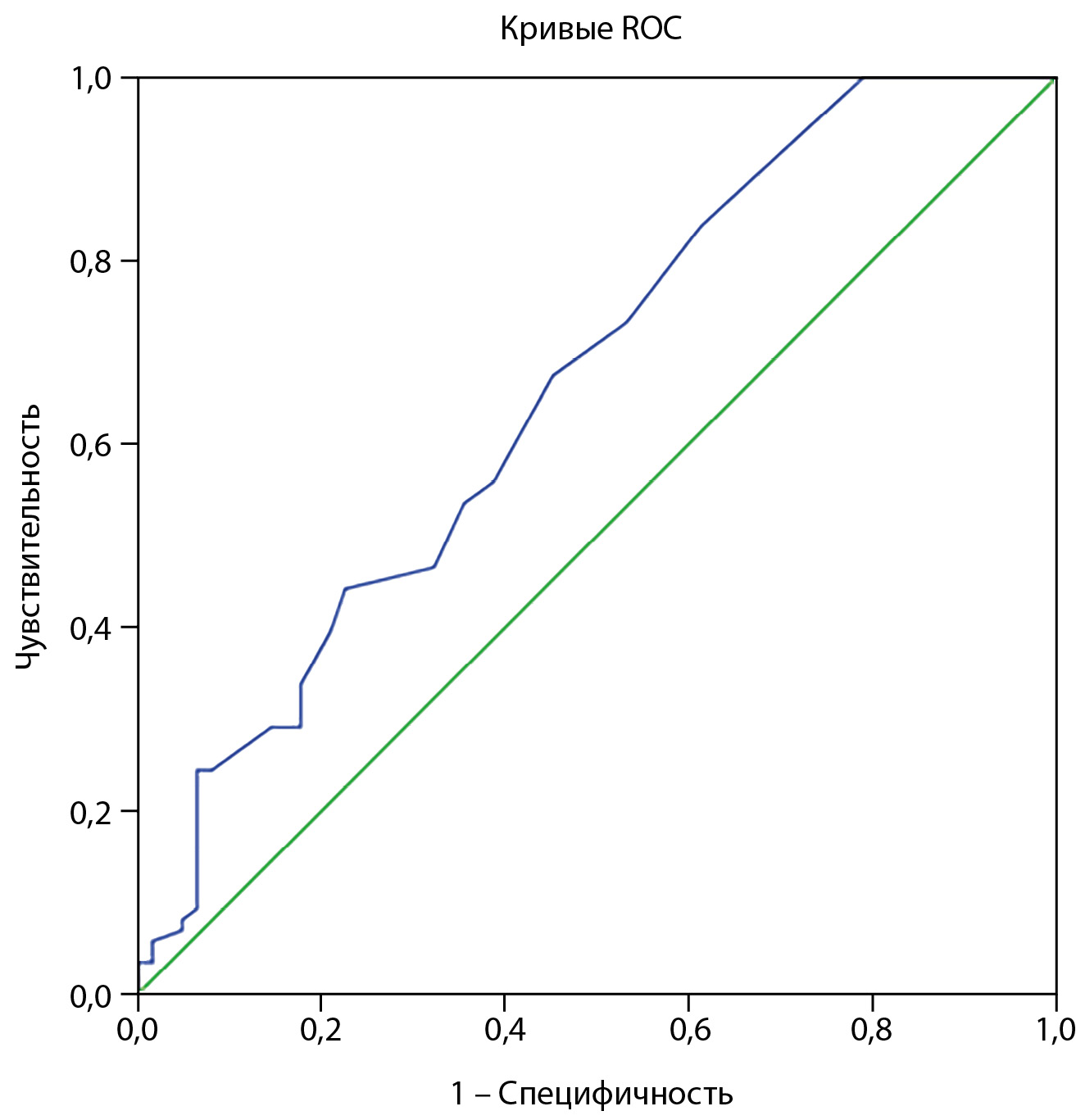
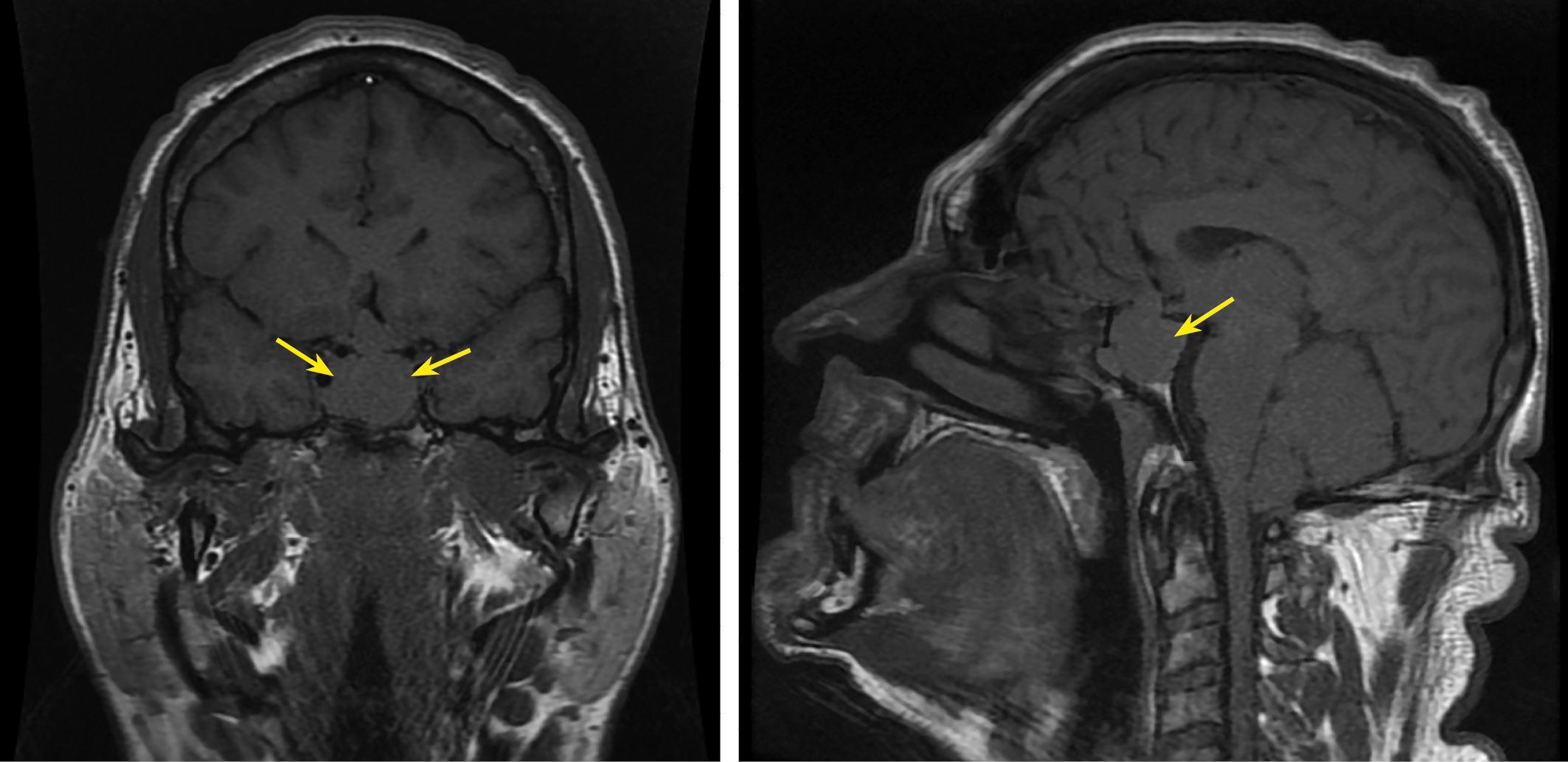
METHODS: An interventional cross-sectional study was conducted at the (Endocrinology Research Center. The study included 90 patients with polyuria-polydipsia syndrome from September 2021 to September 2023. All patients underwent sequential two tests with osmotic stimulation: 3% hypertonic saline infusion test and a water deprivation test. The final diagnosis was established based on the results of a fluid deprivation test, the patient’s anamnestic data (previous operations, diseases of the hypothalamic-pituitary region, the presence of mental illnesses), MRI data (the presence of a hyperintense signal from the posterior pituitary on T1-weighted images, a detected tumor or infiltrative formation of the hypothalamic-pituitary area, presence of Rathke’s pouch cyst).
RESULTS: 48 patients with a final diagnosis of DI and 42 with a final diagnosis of PP were analysed. A cut-off point for urine osmolality during infusion test with 3% hypertonic saline was found: values less than or equal to 377 mOsm/kg support the diagnosis of DI, and values higher than 377 mOsm/kg support the diagnosis of PP. The sensitivity of the criterion is 89%, 95% CI (77%; 97%), specificity — 98% (87%; 100%), PPV — 98% (88%; 100%), NPV — 89% (76%; 96%), accuracy 93% (86%; 98%).
CONCLUSION: The proposed criterion for differential diagnosis has comparable diagnostic accuracy in relation to the differential diagnosis of DI and PP, while the safety of the test may be higher.
BACKGROUND: morphological changes during the pubertal growth spurt can serve as a model for variation in body composition and, in particular, body fat mass (BFM) without any interventions in the human body and associated changes in heart rate variability (HRV).
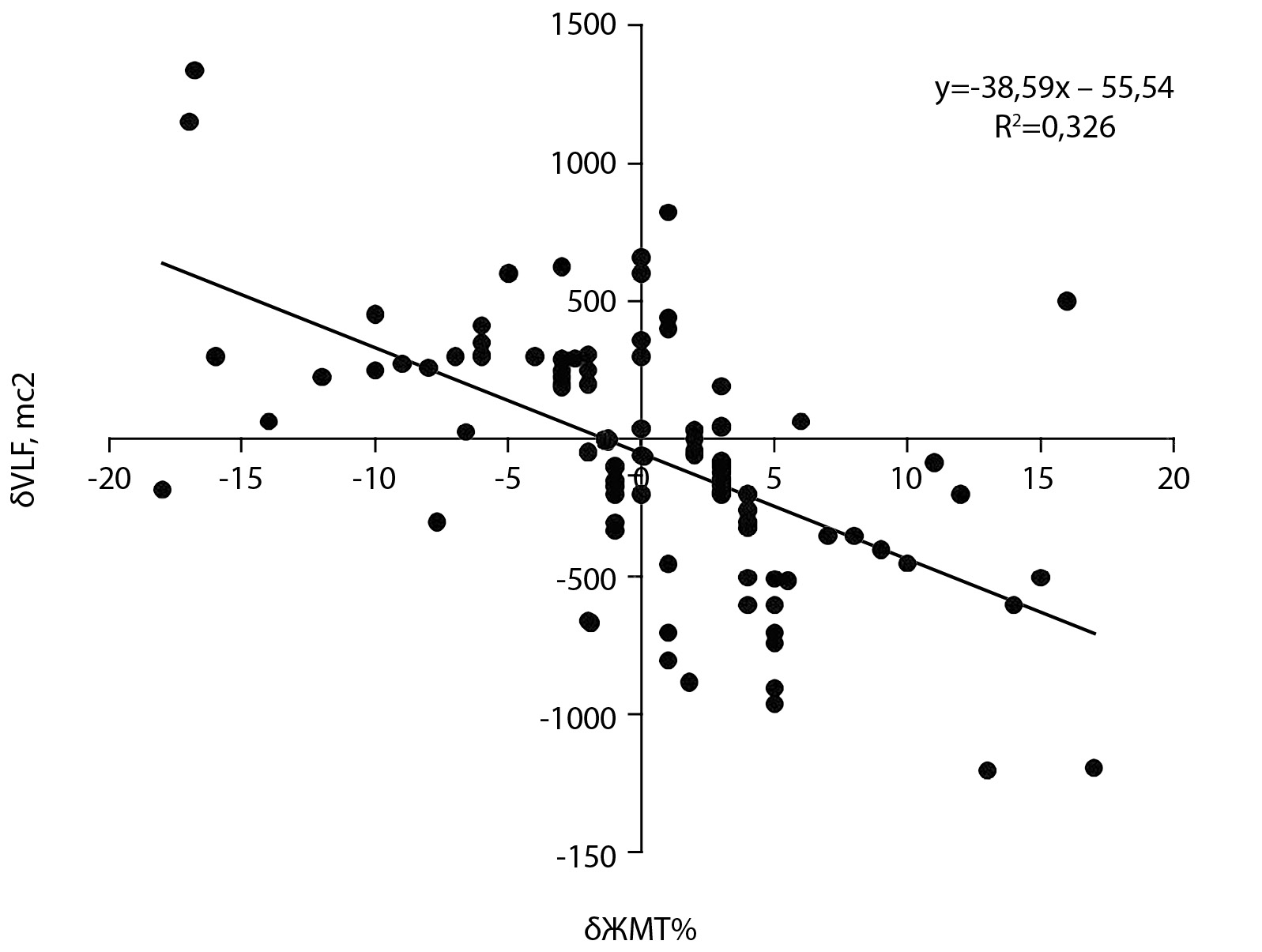
AIM: to study concomitant changes in the VLF spectrum of heart rate variability and body composition in girls during a Two-year study in the age range from 10 to 12 years.
MATERIALS AND METHODS: electrocardiography, anthropometry, bioimpedansometry.
RESULTS: we conducted a three-year open, uncontrolled, non-randomized study-observation of 60 girls in the age range from 10 to 12 years. This age range made it possible to obtain a wide variation in the rate of increase in body fat mass (BFM%) from negative to positive values. The oscillation power of the very low-frequency component (VLF, ms2 and %) in the HR variability increased statistically significantly with decreasing BFM %. In response to an increase in BMT%, reverse changes were observed. The VLF parameter (ms2) is associated with a positive moderate relationship with the basal metabolic rate (BM) at the age of 10 years (r=0.314, p=0.013). At the same age, the BFM % parameter is associated with an average negative relationship with the BM parameter (r=–0.681, p<0.001).
CONCLUSION: in pubertal girls, the change in the composite body composition with a decrease in fat mass is associated with an increase in the absolute (ms2) and relative (%) power of oscillations of the very low-frequency VLF component in HRV.
BACKGROUND: Obesity is a widespread disease associated with serious complications. Obesity is a risk factor for many chronic diseases. The most common type of obesity is polygenic obesity, the pathogenesis of which involves external and internal factors, including genetic ones.
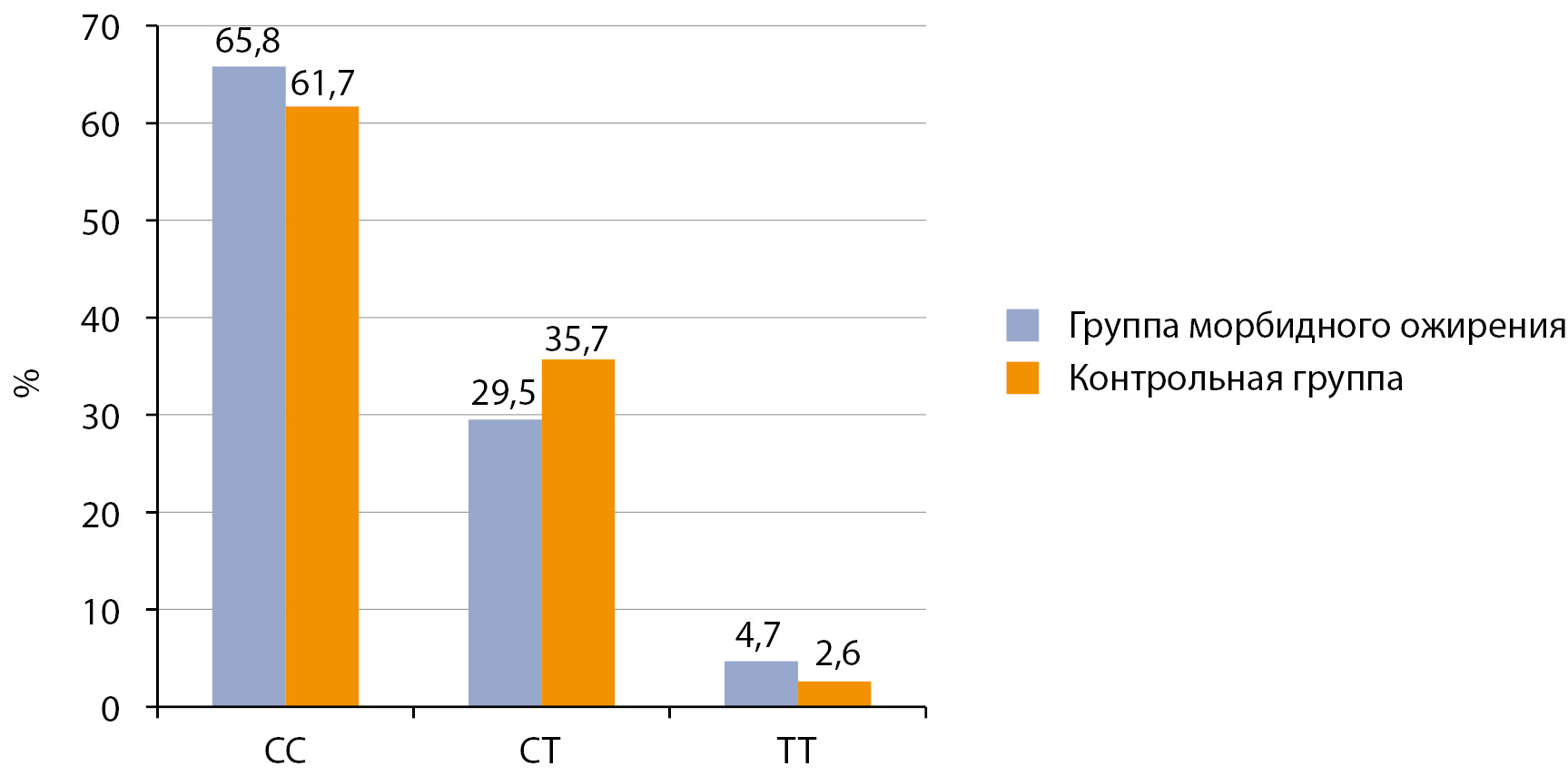
AIM: Search and study of the association of variants of the nucleotide sequence rs9939609 of the FTO gene, rs7903146 of the TCF7L2 gene, rs1799883 of the FABP2 gene, rs1800497 of the DRD2 gene, rs17782313 of the MC4R gene with morbid obesity in women.
MATERIALS AND METHODS: Study design is case-control study. The morbid obesity group and the control group were formed from the DNA bank of participants of the international project HAPIEE. Genotyping was performed by PCR-RFLP and real-time PCR (TaqMan probes, Applied Biosystems, USA). Statistical analysis was performed in SPSS software using Pearson’s chi-square test, Fisher’s exact two-tailed test with Yates’ correction for continuity. The significance level was used p<0.05.
RESULTS: Morbid obesity group included 192 women (mean age 57.02± .16 years) with BMI over 40 kg/m2, control group included 450 women (mean age 55.44±7.41 years) with normal BMI (18.5-24.9 kg/m2). There were no statistically significant differences between the groups in the frequencies of genotypes and alleles rs7903146 of the TCF7L2 gene, rs1799883 of the FABP2 gene, rs1800497 of the DRD2 gene (p>0.05). In the group of morbid obesity, the proportion of carriers of the TT genotype rs9939609 of the FTO gene was statistically significantly lower, and the AT genotype was significantly higher than in the control group (OR=0.579, 95% CI 0.399-0.840, p=0.004; OR=1.408, 95% CI 1.003- 1.976, p=0.047, respectively). The heterozygous TC genotype rs17782313 of the MC4R gene is statistically significantly more common (OR=1.825, 95% CI 1.257-2.652, p=0.002), while the homozygous TT genotype is less common (OR=0.500, 95% CI 0.346-0.723, p<0.001) in group of morbid obesity compared with the control group.
CONCLUSION: Heterozygous genotypes of the rs9939609 of the FTO gene (AT) and rs17782313 of the MC4R gene (TC) are risk genotypes; the homozygous genotype TT of the variants is protective for morbid obesity in women. Single nucleotide variants rs7903146 of the TCF7L2 gene, rs1799883 of the FABP2 gene, and rs1800497 of the DRD2 gene are not associated with morbid obesity in women.
BACKGROUND: True gynecomastia is associated with excess body mass, which is caused by an imbalance of androgens/estrogens. Therefore, there is an interest in evaluating the possibility of drug therapy for this condition through the use of antiestrogens or aromatase inhibitors.
AIM: To evaluate the possibility of drug therapy for true gynecomastia in adult men with excess body mass through the use of clomiphene or letrozole.
MATERIALS AND METHODS: A retrospective study included men with newly developed gynecomastia and excess body mass who sought medical help at the Endocrinology Research Center from January 2020 to May 2024, and received either clomiphene therapy or letrozole for a period of 4 weeks. All patients were evaluated for the condition of their breast glands, total bilirubin, liver transaminases, creatinine, urea, luteinizing hormone, prolactin, sex hormone-binding globulin, estradiol, total testosterone, alpha-fetoprotein, and chorionic gonadotropin. The baseline level of statistical significance was set at p<0.05.
RESULTS: With clomiphene treatment, no statistically significant differences were found in the evaluated parameters, except for estradiol and testosterone levels, which increased. Clomiphene therapy worsened the condition of three patients (13% (95% CI 2,8;33,6)) - they experienced breast pain that was not present at the time of prescription. With letrozole treatment, there was a positive trend - all evaluated parameters significantly improved. Comparing the changes in the studied parameters, it was found that letrozole treatment had a better effect in terms of the severity of gynecomastia (-1[0;-1] degree), reduction in estradiol levels (-31,7[-8,8;-90,8] pmol/l), and also reduced the number of patients willing to undergo surgical removal of gynecomastia (-63,4% (95% CI -46,9;-77,9)).
CONCLUSION: The use of an aromatase inhibitor reduces the severity of gynecomastia and decreases the number of patients willing to undergo surgical removal.
REVIEWS
Obesity is one of the most important health problems. Body weight can be controlled through a combination of a healthy diet and physical activity, but hypertrophic obesity is often complicated by other comorbidities such as type 2 diabetes mellitus (T2DM), cardiovascular disease, hypertension and various forms of arthritis. If intense physical activity is contraindicated for patients, then alternative approaches to combat obesity can be developed. The discovery of beige adipocytes in white adipose tissue has attracted attention to their use as a target for therapy. There are molecules of various origin that are capable of modulating the formation of beige adipocytes by interacting with critical signaling cascades, leading to increased thermogenesis. One such approach would be to stimulate the transition of white adipose tissue cells into more catabolically active beige cells using nutrients and small molecule drugs.
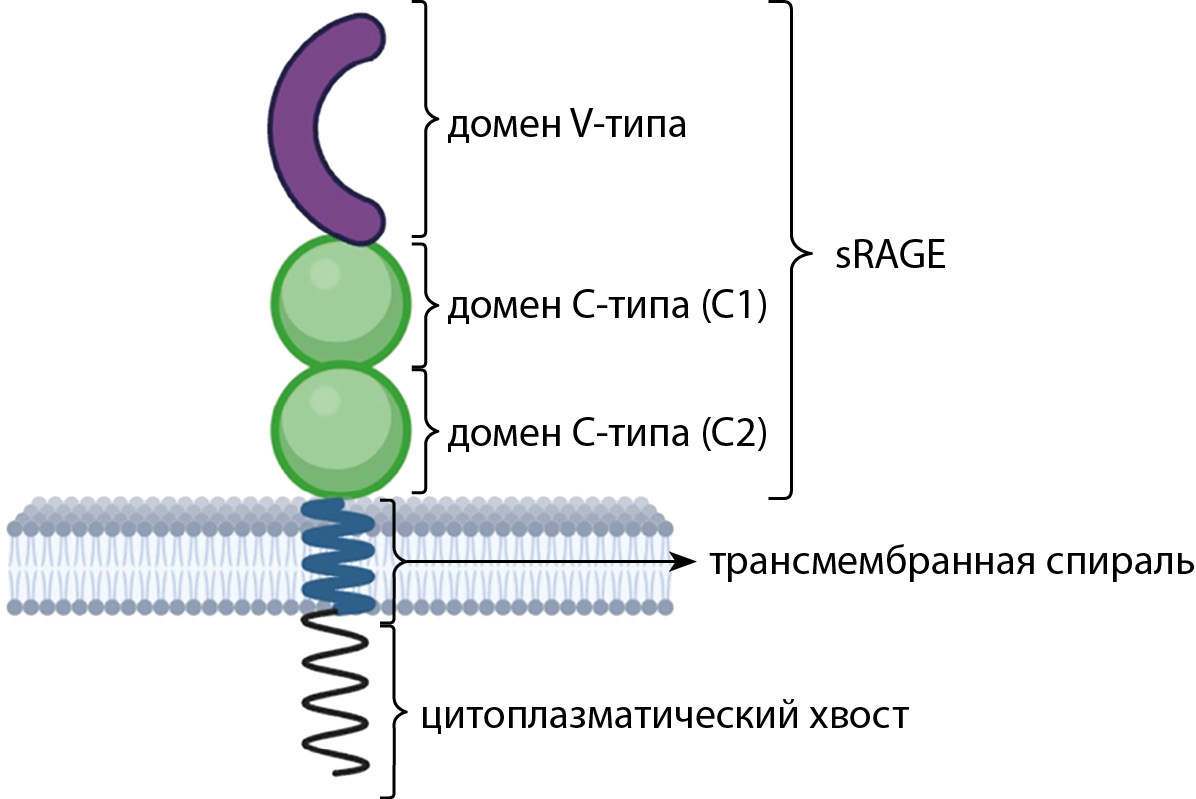
Consuming high-calorie and thermally processed foods leads to increased body weight and increased levels of advanced glycation end products (AGE) in the human body. AGE has been shown to contribute to dietary oxidative stress and processes that play a major role in the development of type 2 diabetes mellitus (T2DM). Data obtained from cellular and mouse models indicate that the interaction of AGEs with their receptor, RAGE (receptor for advanced glycation end products), promotes the development of inflammation in adipose tissue (AT) through the activation of pro-inflammatory signaling cascades. In addition, there is new evidence, which shows influence of RAGE on the transformation of AT macrophages into the provoking M1 phenotype, which also promotes the degree of inflammation in AT. Inflammation in AT leads to the development of insulin resistance and, accordingly, T2DM. At the same time, there are also RAGE isoforms that can prevent the start of the inflammatory process. The review is devoted to modern views on the role of AGE-RAGE systems in the development of carbohydrate metabolism disorders in obese people.
Diabetes mellitus is a chronic disease that requires lifelong medical supervision. Hundreds of millions of people around the world and the rapidly increasing incidence of diabetes are a heavy burden on the health system. Over the past decades, many works have been published on changes in the intestinal microbiota and its permeability in diabetes mellitus of the first and second type (T1DM and T2DM). Due to changes in the permeability of the intestinal wall, its barrier function is also disrupted, as a result of which the access of infectious agents and food antigens to the immune elements of the mucous membrane is facilitated. These pathological changes can eventually lead to immune reactions with damage to pancreatic beta cells, and contribute to an increase in the production of inflammatory cytokines, followed by insulin resistance. Changes in the qualitative and quantitative composition of the microbiota play an important role in the manifestation of many autoimmune and metabolic diseases. Understanding the factors regulating the function of the intestinal barrier and the composition of the intestinal microenvironment provides important information about the interactions between luminal antigens and elements of the immune response. This review analyzes the latest advances in medicine in understanding the mechanisms linking the host organism, the intestinal microbiota and increased intestinal permeability in T1DM and T2DM.
Vitamin D deficiency and insufficiency are widespread globally with multiple factors playing a role in their development. Such as limited exposure to sunlight, poor nutrition, gastrointestinal diseases, and obesity, which affects approximately 39% of the world’s adult population. In addition to its canonical role in skeletal function, vitamin D modulates adipogenesis, insulin secretion, and action in diabetes. Vitamin D deficiency due to obesity is likely due to decreased bioavailability of vitamin D through synthesis in the skin and from dietary sources, which is associated with its deposition in body fat depots. While a direct effect on adipogenesis appears to be realized during critical periods of life (pre- and postnatal periods). Vitamin D directly regulates genes involved pathways of insulin secretion and action. The high worldwide prevalence of vitamin D deficiency may be associated with the high incidence of type 2 diabetes, and normalizing vitamin D levels in patients may be an effective strategy to slow the progression of type 2 diabetes and its complications.
Over the past few decades, obesity has become a growing public health problem worldwide. The goal of fighting obesity is to improve health. Sustained weight loss of more than 10% of the total body weight improves the course of many obesity-related diseases, as well as the quality of life. The high effectiveness of bariatric surgery in the treatment of obesity in achieving significant and sustained weight loss has been demonstrated in several studies. In most centers where bariatric surgery is performed, the recommendation for preoperative weight loss is followed. The enlarged left lobe of the liver makes it difficult to access the stomach and, accordingly, prevents technically correct operation. Weight loss before bariatric surgery reduces the risk of complications in the postoperative period, and therefore preoperative preparation in the form of hypocaloric nutrition and regular physical activity is recommended for patients, considering concomitant pathology. One of the problems in the postoperative period is the need to change the usual lifestyle and diet due to the need to follow the recommendations of the attending physician. This can lead to a decrease in the quality of life after surgery due to psychoemotional overstrain. The nutrition of bariatric patients implies significant changes associated with a decrease in the amount of food consumed, difficulty in assimilation of nutrients, and the poverty of flavors offered up to this day in the specialized nutrition market. With the help of food products within the framework of low-calorie diets, it becomes almost impossible to feed such a patient without reducing their nutritional value. In 2024, balanced low-calorie nutrition OPTIFAST® (OPTIFAST) appeared on the Russian market, which has proven itself worldwide for more than 50 years and has shown its effectiveness and safety in more than 80 international clinical trials with a high level of evidence. OPTIFAST provides the patient with all the necessary nutrients and allows you to manage the daily calorie intake, gives the patient a feeling of satiety necessary for high adherence to a low-calorie diet, which is indicated for patients with obesity and overweight.
CASE REPORT
Acromegaly is a severe neuroendocrine disease characterized by excessive production of the growth hormone (GH). The slow development of symptoms increases the diagnostic search up to 15 years. Permanent effect of the growth hormone on the human body can cause structural and functional disorders of organs. The main complications of acromegaly include cardiovascular, respiratory, and musculoskeletal system dysfunction, as well as impaired carbohydrate metabolism and an increased risk of developing neoplasms.
Often, nonspecific symptoms of acromegaly can be masked by other pathologies or their complications, such as obesity. An increase in subcutaneous fat, increased blood pressure, joint pain, edema, and impaired carbohydrate and lipid metabolism are observed both in acromegaly and in obesity. An additional factor in the development of obesity as a complication of acromegaly is the development of sleep apnea, which triggers a series of pathological processes that ultimately lead to Pickwickian syndrome.
We present a clinical case of a patient with acromegaly and obesity, discussing the effects of excess body weight on the course of the underlying disease, the presence of complications, and an individual approach to treatment.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2306-5524 (Online)