Scroll to:
Daily calcium profile in diagnosis of hypo- and hypercalcemia in patients with chronic hypoparathyroidism. clinical case series
https://doi.org/10.14341/omet12729
Abstract
Hypoparathyroidism is a rare endocrine disorder characterized by hypocalcemia and hyperphosphatemia, due to absent or inappropriately low serum parathyroid hormone (PTH) levels. The chronic postoperative hypoparathyroidism accounts approximately 75% of patients; the genetic, autoimmune or idiopathic forms are significantly less common. Today, chronic hypoparathyroidism remains the last major endocrine deficiency, for which hormonal replacement therapy has not found widespread use. Achieving the target levels of phosphorus-calcium metabolism is an important factor of the disease control, required for the prevention of short- and long-term complications. The standard therapy with active metabolites/analogues of vitamin D (alfacalcidol, calcitriol) and calcium supplements does not always allow to achieve the target treatment goals. Despite high doses of calcium and active vitamin D, some patients suffer from unstable calcium levels and associated symptoms.
The measurement of serum calcium and phosphorus in the early morning hours remains the main laboratory tests for such patients, but in sometimes this diagnostic approach does not really reflect the true picture.
The presented clinical cases describe the changes of both hyper- and hypocalcemia within one day in patients with chronic postsurgical hypoparathyroidism managed by standard therapy.
For citations:
Kovaleva E.V., Eremkina A.K., Mokrysheva N.G. Daily calcium profile in diagnosis of hypo- and hypercalcemia in patients with chronic hypoparathyroidism. clinical case series. Obesity and metabolism. 2021;18(2):175-179. https://doi.org/10.14341/omet12729
BACKGROUND
Hypoparathyroidism is a relatively rare endocrine disorder with the prevalence rate of 23-46 cases per 100 000 population characterized by the diminished function or absence of parathyroid hormone (PTH) [1]. The most frequent cause of the disease is unintentional removal or blood supply disturbance of the parathyroid glands (PTG) during surgical interventions in the neck organs. The long-term course of hypoparathyroidism is associated with risks of developing complications and increased mortality [2]. Metabolites/analogues of vitamin D (alfacalcidol or calcitriol) and calcium supplements (mainly calcium carbonate) are used to treat hypoparathyroidism. According to the 2015 European Society of Endocrinology Clinical Guideline: Treatment of chronic hypoparathyroidism, the treatment is targeted to maintain low-normal calcemia level (2.1-2.3 mmol/L), normophosphatemia and normocalciuria (no more than 6.25 mmol/day for women and 7.5 mmol/day for men) [3]. Achieving the target levels of phosphorus-calcium metabolism is an important factor of the disease control, required for the prevention of short- and long-term complications. The large cohort study (n=431) found that hyperphosphatemia, increased the calcium to phosphorus ratio as well as frequent events of hypercalcemia (1-3 events per year) due to chronic overdose of calcium supplements and vitamin D are associated with higher risks of cardiovascular and infectious diseases, renal impairment and mortality in patients with hypoparathyroidism [2]. At the same time hypocalcemia is also one of adverse factors regarding cardiovascular complications. Hypoparathyroidism «inadequate control» criteria are not established for now. Although, the impact of various parameters on disease complications is being discussed, in particular [4]:
- high dosages of calcium supplements (over 2500 mg/day) and active metabolites/analogues of vitamin D (over 1.5 mcg/day of calcitriol or over 3.0 mcg/day of alfacalcidol); 2. acute symptoms of hypocalcemia (cramps, paresthesia, etc.) in spite of the provided treatment; 3. risk factors and/or complications such as hypercalciuria, nephrolithiasis/nephrocalcinosis, chronic kidney disease of stages 4 and 5. According to the European Clinical Guideline, it is necessary to control phosphorus and calcium metabolism parameters several times per week and at least once in 3-6 months in case of stable disease state. If the laboratory control is not frequent enough, it is possible to miss significant factors of complications development (events of hypo-/hypercalcemia, hyperphosphatemia) that aggravates the long-term prognosis for this cohort of patients. Nevertheless, this frequency of laboratory tests in some cases may not be enough. Calcium level measurement in the early morning hours remains the main laboratory test. However, morning levels do not always show the true situation with calcemia during the day which is first of all related to different pharmacokinetics of medicines used to treat hypoparathyroidism. It is especially relevant for patients who still have specific complaints though the levels of calcium in the blood serum reached the target during standard morning tests. In this case, it seems more appropriate to measure the daily calcium profile. The clinical cases presented below describe alternations of hyper- and hypocalcemia events within one day in patients with chronic postsurgical hypoparathyroidism.
CASE DESCRIPTION
Clinical case 1.
Female patient, L., 18 y.o., was admitted at the Department of Parathyroid Glands Pathology (DPTGP) of the Endocrinology Research Centre with complains of occasional numbness of fingers, jerking and spasms of extremities muscles and anterior abdominal muscles that mostly occurred in the evening and at night. From the medical history we know that persistent hypoparathyroidism developed after the surgical of Graves’ disease (PTH is 7.11 pg/ml, reference interval (RI) is 15-65). At admission she received the following treatment: alfacalcidol — 2.5 mcg/day (1.25 mcg in the morning (9:30) and in the evening (19:00)), levothyroxine sodium — 125 mcg/day. The lab findings showed the target values of calcium (albumin-adjusted blood calcium — 2.33 mmol/L, RI — 2.15-2.55), phosphorus (1.29 mmol/L, RI — 0.74-1.52) combined with moderate hypercalciuria of up to 8.6 mmol/day (RI — 2.5-6.5). The level of 25 (OH) vitamin D confirmed with deficiency — 15.4 ng/ml (RI — 30-100). Hypothyroidism was compensated (thyroid-stimulating hormone (TSH) — 1.69 mIU/L, RI — 0.43-4.2). The screening was conducted to check for hypoparathyroidism complications. Kidney US was without pathological findings. Kidneys preserved their filtration function (estimated glomerular filtration rate (e-GFR) CKD-EPI: 116 ml/min/1.73 m2). The ophthalmologist did not find data suggestive of cataract.
Taking into account specific complaints and to adjust the treatment the patient’s daily calcium profile was assessed (to determine total and albumin-adjusted calcium every 2h within a day). The test findings allowed for the first time to note hypercalcemia events of up to 2.8 mmol/L of total calcium (2.66 mmol/L of albumin-adjusted calcium) during the day and hypocalcemia events of down to 2.0 mmol/L of total calcium (1.94 mmol/L of albumin-adjusted calcium) in the early morning (fig. 1).
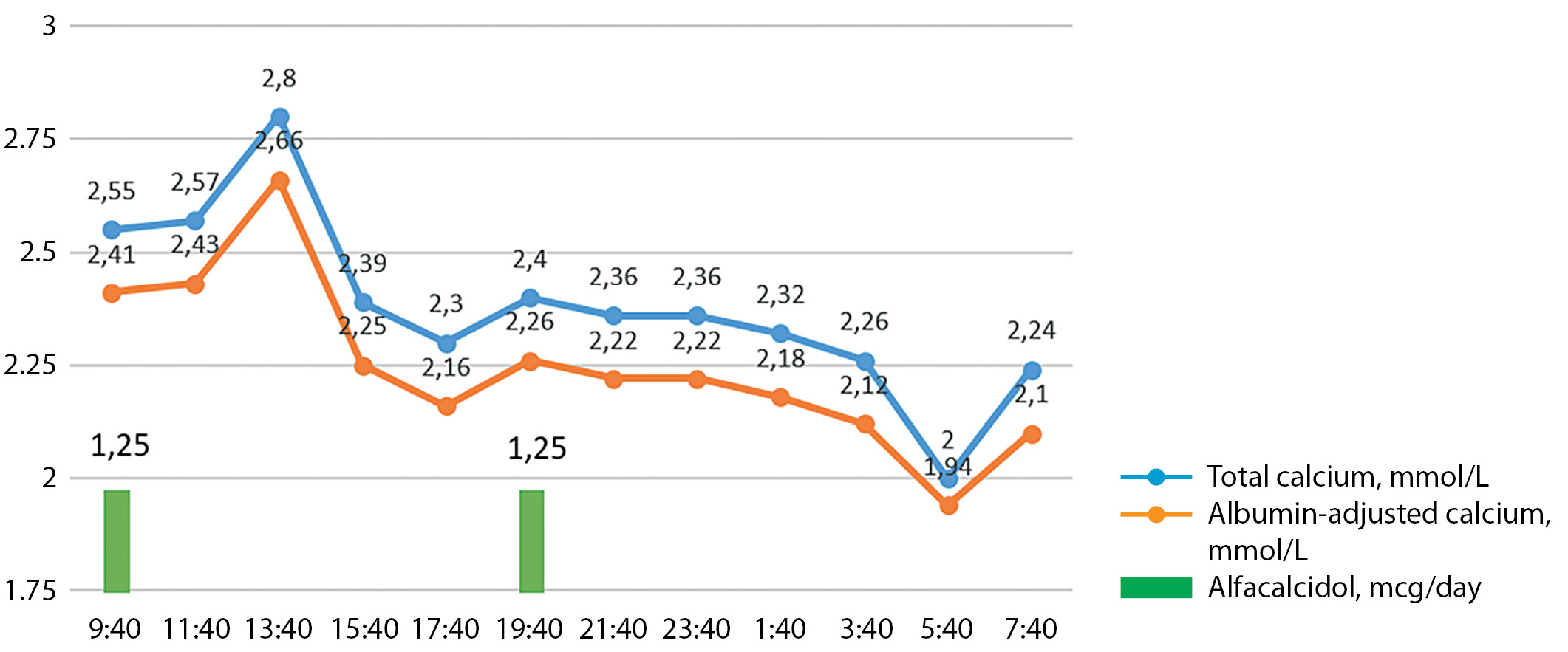
Figure 1. Calcium daily profile in patient L.
Considering the results of the calcium daily profile and non-target calcium values in the daily urine, the patient was recommended to decrease alfacalcidol down to 2 mcg per day with the daily dosage split: 0.5 mcg in the morning and middle of the day and 1 mcg at bedtime. To compensate for vitamin D deficiency colecalciferol was administered in the saturating dose of 7000 IU per day for 8 weeks with the transition to the maintaining dose of 2000 IU per day.
Clinical case 2.
Female patient, S., 47 y.o., was admitted at the DPTGP with complaints of numbness, tingling, formication in fingertips and tiptoes, on the face; decrease in visual acuity, blurry vision; palpitations, heart dysfunction. Postsurgical hypoparathyroidism was diagnosed after the surgical treatment of multinodular euthyroid goiter in April 2016. In the early post-surgical period seizure syndrome developed, there was decrease of total calcium level down to 1.89 mmol/L (ionized calcium — 0.84 mmol/L, RI — 1.03-1.23), PTH level was not studied. Alfacalcidol was administered in dosage of 2 mcg/day, and calcium carbonate 1500 mcg/day.
Then as hypocalcemia persisted (total calcium — 1.95 mmol/L), alfacalcidol dose was increased up to 3-3.5 mcg/day; as daily calciuria had non-target values (9.07 mmol/day), hydrochlorothiazide was also added to the treatment — 25 mg/day.
The first hospitalization to the DPTGP was in January 2019. The examination confirmed the chronic character of postsurgical hypoparathyroidism (PTH — 5.75 pg/ml) in subcompensation (albumin-adjusted calcium — 1.98 mmol/L, phosphorus — 1.53 mmol/L, calcium in daily urine — 8.19 mmol/day). Kidney US detected a small stone up to 3 mm. The hydrochlorothiazide dose was increased up to 50 mg/day.
Follow-up showed that paresthesia and jerking complaints persisted, lab tests showed persisting mild hypocalcemia (2.04-2.0-1.98 mmol/L) and moderate hyperphosphatemia (1.69 mmol/L) in spite of quite high dosage of the standard therapy. There was an attempt to switch the patient to calcitriol, but this medication caused severe pains in the epigastric region, thus it was canceled.
The hydrochlorothiazide dose was decreased down to 12.5 mg/day and later all the way down to the full withdrawal due to the associated hypotension.
The last hospitalization to the DPTGP was in February, 2021 with all the complaints mentioned above. When admitted, the patient got the following treatment: levothyroxine sodium — 75 mcg in the morning, alfacalcidol — 3 mcg/day, colecalciferol — 2500 IU/day. The lab findings showed the normocalcemia (albumin-adjusted blood calcium — 2.33 mmol/L), moderate hyperphosphatemia (1.57 mmol/L), hypercalciuria of up to 12.08 mmol/day. The level of 25 (OH) vitamin D conformed with insufficiency — 28.8 ng/ml. Hypothyroidism was compensated (TSH — 1.06 mIU/L). Given the clinical and laboratory data the patient’s daily calcium profile was assessed (fig. 2). The persistent increase of blood calcium level was detected during the day: from moderate (2.64 of total calcium, 2.56 mmol/L of albumin-adjusted calcium) to severe hypercalcemia (2.85 of total calcium, 2.77 mmol/L of albumin-adjusted calcium).
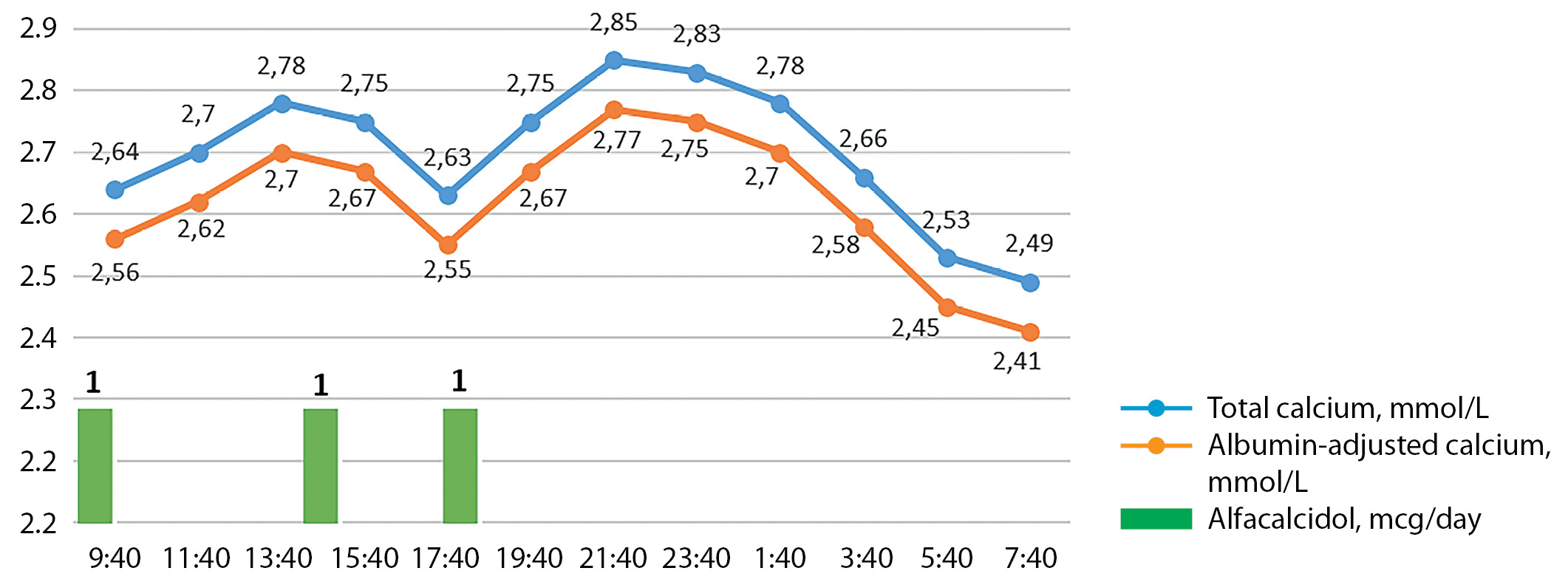
Figure 2. Calcium daily profile in patient S.
In this case hypercalcemia in the patient with hypoparathyroidism was caused by alfacalcidol overdose which could have not be diagnosed previously as the serum calcium level in the early morning stayed targeted (calcemia is minimum at 07:40-09:40 during the day — 2.49 mmol/L of total calcium and 2.41 mmol/L of albumin-adjusted calcium). These results also explain the presence of hypercalciuria in the patient as it is known that high blood calcium values inevitably lead to its increased excretion through kidneys.
Thus, in this case the abundance of complaints could have been partially associated with hypercalcemia secondary to alfacalcidol overdose. At the Unit the drug dosage was reduced down to 2.5 mcg per day and follow-up blood and urine lab control was recommended. To manage the concomitant vitamin D deficiency, colecalciferol was administered in the dose of 7000 IU/day for 4 weeks with the transition to the maintaining dose of 2000 IU per day in 1 month.
We cannot exclude that the persistent symptoms could have been the result of the psychosomatic reaction of fixating at the physical state with already known and expected disease manifestations what was confirmed by the neuropsychiatrist examination.
DISCUSSION
Some cases of severe hypercalcemia associated with vitamin D and calcium supplements overdose are described in patients with hypoparathyroidism, including in presence the use of dihydrotachysterol (increase of total calcium values up to 3.7-4.97 mmol/L) [5][6] and alfacalcidol (increase of total calcium values up to 4.26 mmol/L) [7]. There is also data about the development of the milk-alkali syndrome in patients with chronic hypoparathyroidism who receive high doses of calcium supplements [8][9]. In both clinical cases, we presented daily profiles of patients with chronic postsurgical hypoparathyroidism treated with alfacalcidol. Although the treatment allowed to reach the target calcium and phosphorus values in the early morning, the daily calcium profile showed chronic overdose with this drug.
Knowledge of pharmacokinetics of administered medication is important. After intake alfacalcidol is fully absorbed in the small intestine, the maximum concentration in plasma is reached in 8-18 h, the circulating half-life is 3 h. Thus, to maintain a smoother peakless calcemia profile in patients with chronic hypoparathyroidism, it is recommended to spread the daily dose over a day.
The physiological PTH release has circadian character, the blood calcium level is unstable during the day and has periods of maximum and minimum values. In that way, the serum calcium level is maximum in the evening (around 20:00) and minimum at night (02:00-04:00) [10] which conforms with PTH release stages.
Patients with hypoparathyroidism do not have the circadian rhythm of PTH and normocalcemia is maintained by regular intake of medication and calcium-enriched food.
The decrease of calcium level in the evening and at night is caused by the lack of medication intake; and in such conditions, the later intake of the evening dose may be a solution.
When managing patients with hypoparathyroidism, it is necessary to actively detect not only hypocalcemia symptoms (cramps, paresthesia, muscular hypertonia), but also the time when these symptoms occur which will allow to personalize the treatment to maintain the stable calcium level during the day. To exclude the concomitant psychosomatic component consultations with other specialists may be required, including neuropsychiatrist.
The determination of disease control should be personalized and defines the management and frequency of follow-up. Our colleagues suggested that the following characteristics significantly impact the disease compensation patients with chronic hypoparathyroidism (fig. 3) [4].
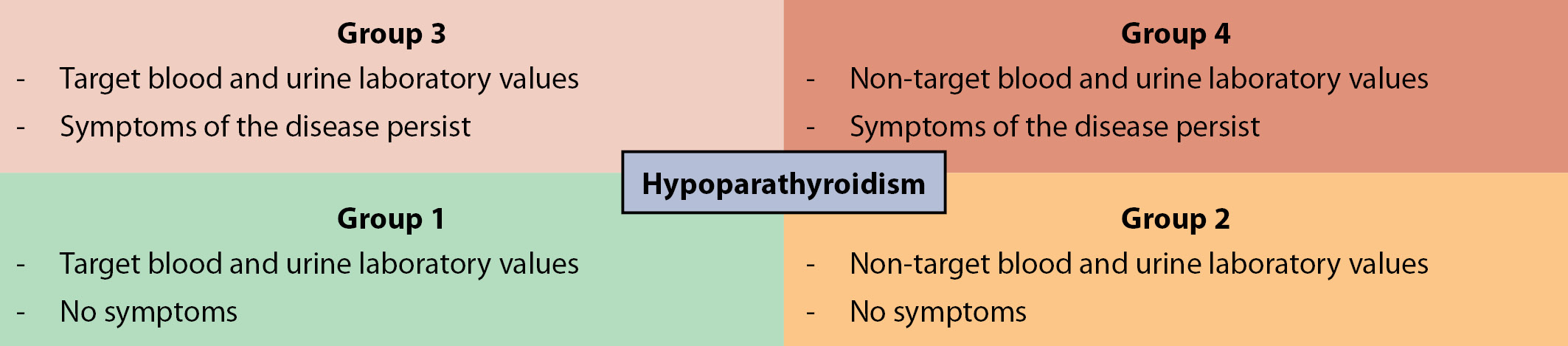
Figure 3. Characteristics of groups of patients with hypoparathyroidism as a function of disease compensation level and presence of comorbidities (based on Iqbal K. et al., 2019 [4]).
CONCLUSION
Today, chronic hypoparathyroidism remains the last major endocrine deficiency, for which hormonal replacement therapy has not the spread use.
To maintain target characteristics of phosphorus and calcium metabolism during the day the standard treatment uses active metabolites/analogues of vitamin D and calcium supplements. This treatment cannot compensate for all PTH actions and is associated with risk of developing complications, in particular, renal impairment. The management of patients with chronic hypoparathyroidism requires a personalized approach from endocrinologists both for diagnosis, including calcium daily profile use, and choice of drug regimen and active follow-up.
ADDITIONAL INFORMATION
Funding sources. The study had financial support of the Russian Foundation for Basic Research within project 19-315-90039.
Conflict of interest. The authors declare no obvious and potential conflicts of interest related to the publication of this article.
Contribution of authors. Elena V. Kovaleva — data acquisition and analysis and findings interpretation, material editing of the manuscript to increase the article scientific value; Anna K. Eremkina — data acquisition and analysis and findings interpretation, material editing of the manuscript to increase the article scientific value; Natalia G. Mokrysheva — significant contribution into the study concept and design, material editing of the manuscript to increase the article scientific value. All of the authors approved the final version of the article before publication, agreed to be responsible for all aspects of the work, implying proper examination and resolution of issues relating to the accuracy or integrity of any part of the work.
Informed consent. The patients signed the informed consent to the publication of personal medical information in an anonymized form.
References
1. Maeda S.S. et al. Diagnosis and treatment of hypoparathyroidism: a position statement from the Brazilian Society of Endocrinology and Metabolism // Arch. Endocrinol. Metab. 2018. Vol. 62, № 1. P. 106–124.
2. Underbjerg L., Sikjaer T., Rejnmark L. Long-Term Complications in Patients With Hypoparathyroidism Evaluated by Biochemical Findings: A Case-Control Study // J. Bone Miner. Res. 2018. Vol. 33, № 5. P. 822–831.
3. Bollerslev J. et al. European Society of Endocrinology Clinical Guideline: Treatment of chronic hypoparathyroidism in adults // Eur. J. Endocrinol. Bristol, UK: Bioscientifica Ltd, 2015. Vol. 173, № 2.
4. Iqbal K. et al. Defining the Characteristics of Chronic Hypoparathyroidism Not Adequately Controlled on Conventional Therapy: Consensus Findings of Three European Delphi Panels. // Adv. Ther. 2019. Vol. 36, № 11. P. 3007–3016.
5. Jensterle M. et al. Dihydrotachysterol intoxication treated with pamidronate: a case report // Cases J. 2010. Vol. 3, № 1. P. 78.
6. Quack I. et al. Dihydrotachysterol therapy for hypoparathyroidism: consequences of inadequate monitoring. Five cases and a review. // Exp. Clin. Endocrinol. diabetes Off. journal, Ger. Soc. Endocrinol. [and] Ger. Diabetes Assoc. Germany, 2005. Vol. 113, № 7. P. 376–380.
7. Tingsarat W. et al. Hypercalcemic Crisis in a Patient with Post-Surgical Hypoparathyroidism // Case Rep. Endocrinol. / ed. Isozaki O. Hindawi, 2019. Vol. 2019. P. 3503651.
8. Somani S., Kotwal N., Upreti V. An unusual case of hypercalcemia in a patient of concomitant hypoparathyroidism and celiac disease. // Clinical cases in mineral and bone metabolism : the official journal of the Italian Society of Osteoporosis, Mineral Metabolism, and Skeletal Diseases. 2016. Vol. 13, № 1. P. 51–53.
9. Skwarek A. et al. Milk-alkali syndrome (MAS) as a complication of the treatment of hypoparathyroidism - a case study. // Endokrynol. Pol. Poland, 2018. Vol. 69, № 2. P. 200–204.
10. Jubiz W. et al. Circadian rhythm in serum parathyroid hormone concentration in human subjects: correlation with serum calcium, phosphate, albumin, and growth hormone levels // J. Clin. Invest. The American Society for Clinical Investigation, 1972. Vol. 51, № 8. P. 2040–2046.
About the Authors
E. V. KovalevaRussian Federation
Elena V. Kovaleva, MD; eLibrary SPIN: 7387-6791.
11 Dm. Ulyanova street, 117036 Moscow
Competing Interests:
not
A. K. Eremkina
Russian Federation
Anna K. Eremkina, MD, PhD; eLibrary SPIN: 8848-2660
Moscow
Competing Interests:
not
N. G. Mokrysheva
Russian Federation
Natalia G. Mokrysheva, MD, PhD; eLibrary SPIN: 5624-3875
Moscow
Competing Interests:
not
Supplementary files
|
|
1. Figure 1. The daily calcemia profile in patient L. | |
| Subject | ||
| Type | Исследовательские инструменты | |
View
(186KB)
|
Indexing metadata ▾ | |
|
|
2. Figure 2. The daily calcemia profile in patient S. | |
| Subject | ||
| Type | Исследовательские инструменты | |
View
(204KB)
|
Indexing metadata ▾ | |
|
|
3. Figure 3. Characteristics of groups of patients with hypoparathyroidism, depending on the degree of compensation of the disease and the presence of concomitant comorbid diseases. | |
| Subject | ||
| Type | Исследовательские инструменты | |
View
(182KB)
|
Indexing metadata ▾ | |
Review
For citations:
Kovaleva E.V., Eremkina A.K., Mokrysheva N.G. Daily calcium profile in diagnosis of hypo- and hypercalcemia in patients with chronic hypoparathyroidism. clinical case series. Obesity and metabolism. 2021;18(2):175-179. https://doi.org/10.14341/omet12729

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).










































